The Week in Research Review, etc 9-24-18
Hey everyone, another great week of rehab-related posts that brought a lot of topics together. The week in research review for 9-24-18 involved:
- Blood Flow Restricted Resistance study
- RTP following an ACL
- Prevalence of knee osteoarthritis in pain-free people
- Training your core
- Dosing Low load Long Duration
- Using Boditrak during the deadlift
Blood Flow Restricted Resistance Exercise as a Post-Orthopedic Surgery Rehabilitation Modality: A Review of Venous Thromboembolism Risk JOSPT Bond et al 2018.
This paper is more of a review of the literature (so be cautious) but raises some important questions and thoughts about #BFR usage in our typical orthopaedic setting.
They talk about important decisions and concepts to be made including precautions, contraindications, and dosage.
They also admit that there are no universally agreed upon standards indicating which post-surgical orthopedic patients may perform BFR safely.
They also list close to 40 different precautions or contraindications including:⠀
❇️Age >40 yr⠀
❇️Creatine Supplement Use ⠀
❇️Diabetes⠀
❇️General/Local Infection ⠀
❇️Hypertension⠀
❇️Immobility >48 hr in the Past Month⠀
❇️Open or Unhealed Soft Tissue Injuries ⠀
❇️Amongst many others
Seems like a pretty strict list but curious to hear what others are using to determine if their client is appropriate for BFR resistance training.
💪🏼Thanks @kieferlammi for the swole session!
Let’s discuss below… tag a colleague who may be interested in discussing…thanks!
Return to Play after ACL
I posted this the other day on #Twitter because I keep hearing people talk about the failure rates after an ACL.
I feel like 1 major reason why people are failing within the 1st 1-2 years after returning is that they get back on the field with residual weakness.
When the patient’s insurance runs out, they workout on their own or often seek out a personal trainer to help them.
I feel we as PT’s can do a much better job at showing our value to our patients by keeping them under our care an progressing them back to their sport.
If we don’t have the facilities to do this, then we must work with others in our region to help our clients get the best care possible.
At @championptp, we often get referrals from area clinicians asking to take over their client’s care and advance them back to their sport. I definitely respect that clinician for recognizing their care may not be the best for the client at that time in the rehab process.
Do you utilize clinicians in your area in these situations? Do you think we could improve our ACL outcomes if we did this more?
Let’s discuss this below and make sure we have a plan in place when that 2-3 month rehab phase approaches. Tag a friend who may benefit from this post…thanks!⠀⠀
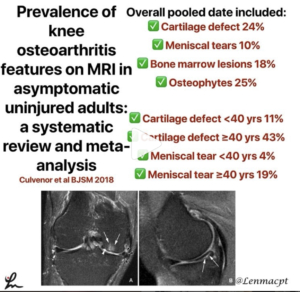
Prevalence of knee osteoarthritis features on MRI in asymptomatic uninjured adults: a systematic review and meta-analysis Culvenor BJSM 2018
This paper ‘performed a systematic review with meta-analysis to provide summary estimates of the prevalence of MRI features of osteoarthritis in asymptomatic uninjured knees.
They basically looked to determine the normal changes in the knee that may be diagnosed on an MRI in people less than and greater than 40 years of age.
The information may help clinicians educate their patients prior to getting an MRI.
Overall pooled date included:⠀
Cartilage defects was 24%⠀
Meniscal tears was 10%⠀
Bone marrow lesions 18% ⠀
Osteophytes 25%⠀
Cartilage defect <40 years 11%⠀
Cartilage defect ≥40 years 43%⠀
Meniscal tear <40 years 4% (seems low to me)⠀
Meniscal tear ≥40 years 19%⠀
Interesting stuff that you need to store in our mental database for future clients.
What do you think of this data? Will it help you in your decisions with your clients?
Tag a friend or colleague who may benefit from this information…thanks!⠀
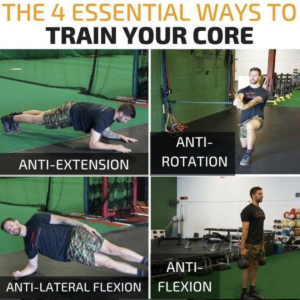
4 WAYS YOU SHOULD BE TRAINING YOUR CORE
Great post by our strength coach @kieferlammi discussing the 4 ways to train your ‘core’. Simple yet a great view of the concepts needed to best address a client’s weaknesses. Give him a follow and see his original post below. @championptp
There are a million different exercises to train your abs/core/trunk/whateveryouwanttocallit. Regardless of which you choose, in my mind there are 4 staple ways that I think belong in every training program:
⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀
1️⃣Anti-Extension – These consist mainly of plank variations, Rollouts, Fallouts, etc.
2️⃣Anti-Rotation – The anti-rotation press or “Pallof Press” is the most popular of this category and can be done from a variety of stances with a variety of tools.
3️⃣Anti-Lateral Flexion – Side planks and unilateral load carries are king here, but this would include anything resisting side bend.
4️⃣Anti-Flexion – Loaded carries and Deadlifts are the top two in my mind, but anything where you have to work to avoid rounding forward, will do.
What are your staples? Anything I’m missing? Disagree? Comment below!
LLLD DOSING
What dosing should you prescribe your patient with a stiff joint when using low load long duration stretching? 🤔
That’s the million dollar question and very little is known.
The one paper that I’m aware of is more of a concepts paper but has been the guidance for my LLLD dosing.
McClure et al talk about 60 minutes per day of total end range of motion time or TERT.
Basically, I tell my clients to apply some form of over-pressure 4x per day for 15 minutes each session. I’ll sometimes do 3x 20 minutes/day if they don’t have the time at work or school.
It allows them to moderately stress the tissue but not take up too much of their time during the day.
The key to this form of stretching (we think) is to elongate the tightened collagen that is limiting the posterior capsule of the knee… see Zhou et al 2018 MSSE ‘Range of Extension Correlates with Posterior Capsule Length after Knee Remobilization.’
Check out this paper and consider this dosing as the basis for your future clients. Do you have any dosing schedules that you use or any research that specifically talk about this?
Let’s talk it out and hopefully help you dose your patients who are tight after knee or elbow surgery…thanks!⠀
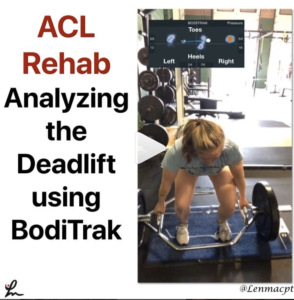
Using Boditrak during the deadlift
This video was recently taken of my #ACL patient who is ~ 12 weeks s/p L ACL reconstruction with a patella tendon autograft and a medial meniscus repair.
I took this video (it’s a mirror image so don’t get confused) to analyze her weight distribution between the involved leg (Left) and the uninvolved leg (right).
As you can see, she spends a lot of time on the front part of her foot throughout much of the deadlift and has her weight shifted to the uninvolved side during her initial pull.
As she ascends up and reaches the max pull position, she is able to redistribute her weight more evenly between each side but continues to keep her weight more toward her toes on that involved side.
To me, I would like to see her weight distribution more equal side to side but also more towards the mid-portion of her foot during the pulling phases.
She self-admits that she is shifting her weight and can’t help it. Through the naked eye, you may be able to see the shift but not necessarily see the anterior/posterior weight distribution (toes/heels).
I like to use the @boditraksports to pick up little nuances and help give feedback to the client.
Did you notice anything else with this video? What would you critique (be nice!!)?
Tag a friend or colleague who may want to see this video and help @lms651 get back to her fencing competitions…thanks!
⠀






Leave a Reply
Want to join the discussion?Feel free to contribute!