Simplifying ACL Rehab
ACL surgery continues to be a huge focus in the literature and in our outpatient rehabilitation settings. Numerous studies focus on return to play guidelines and retear rates. Social media is all over the place, most times. Let’s try to make things simple and set the stage early.
Paralysis by Analysis- What ACL tests are best for return to play
I previously wrote about return to play guidelines here and even the neurocognitive challenges that are associated with ACL rehabilitation.
As troubling as it all seems, I almost feel as if the recent research is confusing and often unattainable in a traditional outpatient PT setting. I’m worried about the paralysis by analysis mindset that seems to have overtaken my recent discussions on social media.
Most don’t have an isokinetic device to test.
Hop tests, vertical jump, strength…what really matters?
Do hop tests really give us a complete picture of an athlete’s return to play readiness?
What combinations of tests are appropriate?
Is it more than just quadriceps strength?
What about a vertical jump test to determine lower extremity strength and function for an LSI?
Lots of questions!
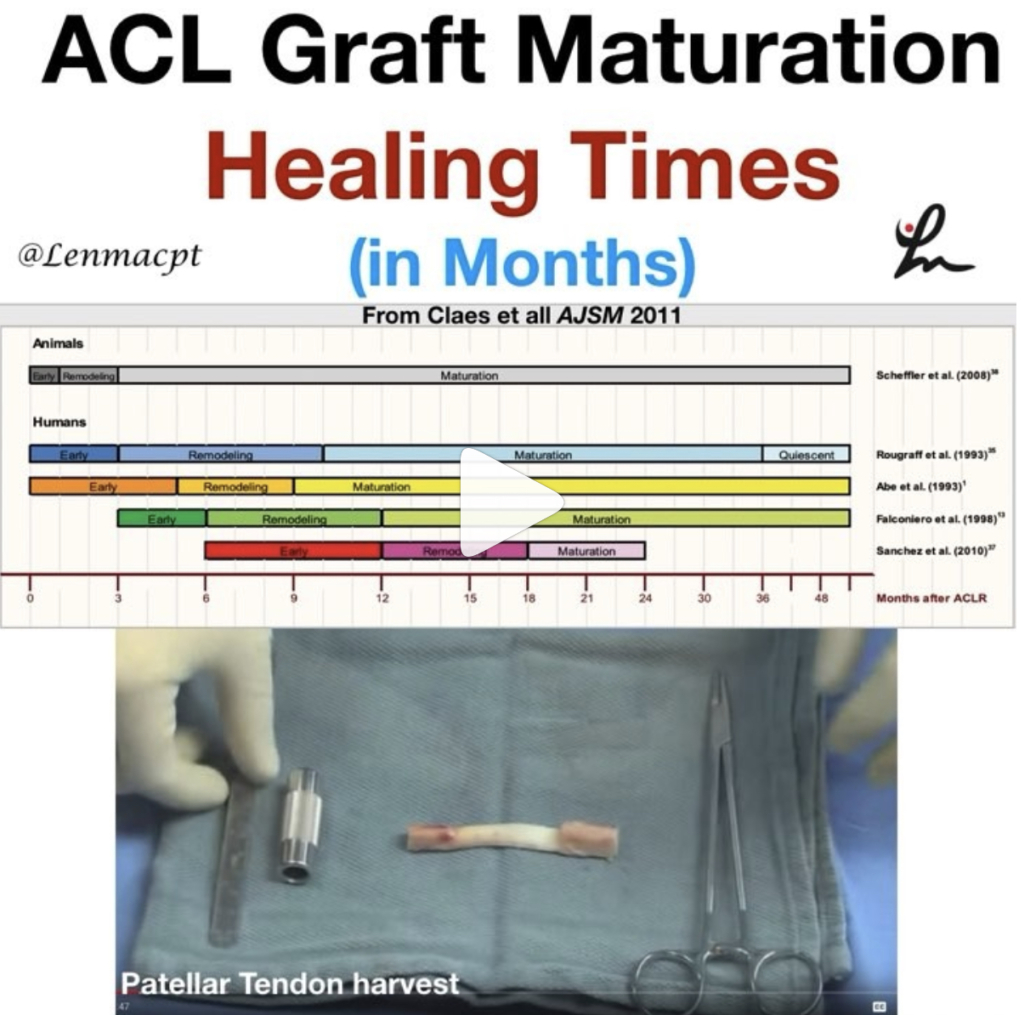
Timeframes have shifted from a 4-6 month return to play goal to a more realistic 9+ months before we return people. Studies continue to show that a slower rehab may be better.
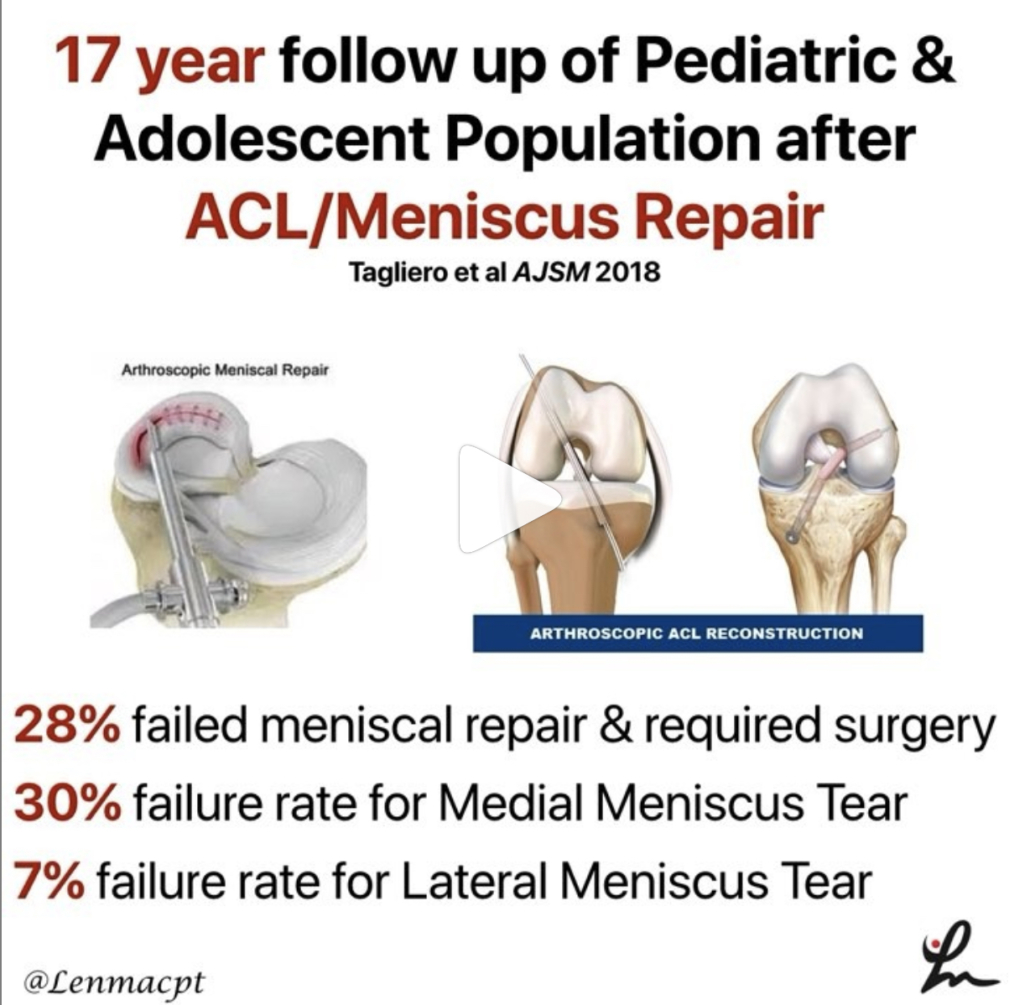
ACL retear rates still too high
Yet, our retear rates still remain very high and we’re still missing the boat for many.
I get it. It’s not just the timelines and rehab. Many are limited by equipment, insurance limitations, differing MD protocols, and so much more. It’s easy to blame one concept when it truly is multifactorial.
That’s why I employ a very simple approach to my ACL rehab programs that seems to work for most and hope this concept can help you too.
It all really occurs at the beginning of rehab when you set the stage for the rest of your planning. If you can establish full motion, remove most of the swelling and restore a pretty normal gait, then you have achieved your goals.
From here, it gets fun and we’ll talk about that later…
An easier approach to ACL rehab
Immediately Post-op Phase
During the earlier stages of rehab, we’ll call it 6 weeks post-op, my main focus is calming the knee down and establishing a normal range of motion.
Range of Motion
It is critical to get the knee as straight as possible and as quickly as possible. For example, most people naturally have some 3-5 degrees of hyperextension. For these individuals, I like to get 0-3 degrees of hyperextension immediately and allow the rest to come through normal functional stresses.
For hypermobile patients, say 10-15 degrees of knee hyperextension, I will only get about 5-7 degrees of hyperextension because I know their underlying tissue mobility will allow the motion to return very easily.
These individuals will not struggle with ROM and it often comes too easily. I don’t want to put unneeded stress on the graft.
Before you yell at me that knee extension will affect retear rates, a study in AJSM showed that the degree of hyperextension did not affect graft laxity and retear rates.
For flexion ROM, I like to have them seated at the edge of the table as I have shown in this video.
I just feel as if it’s easier on the patient and their knee instead of supine or prone, as I’ve described in the video.
I’m a bit obsessive with measuring ROM early, especially extension. It’s critical to stay on top of it and monitor for subtle changes in the motion and end-feel. Here’s an example of an ACL patient of mine who I recently saw and her post-session ROM.
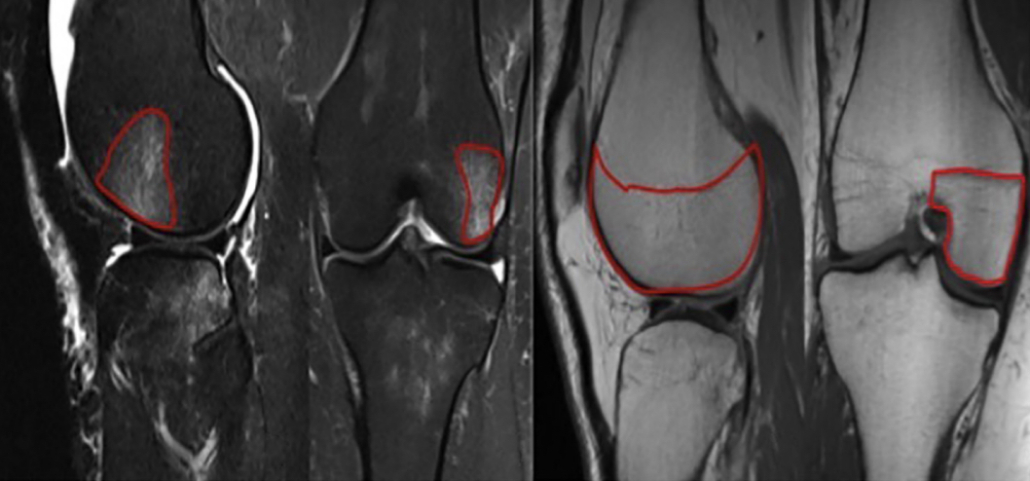
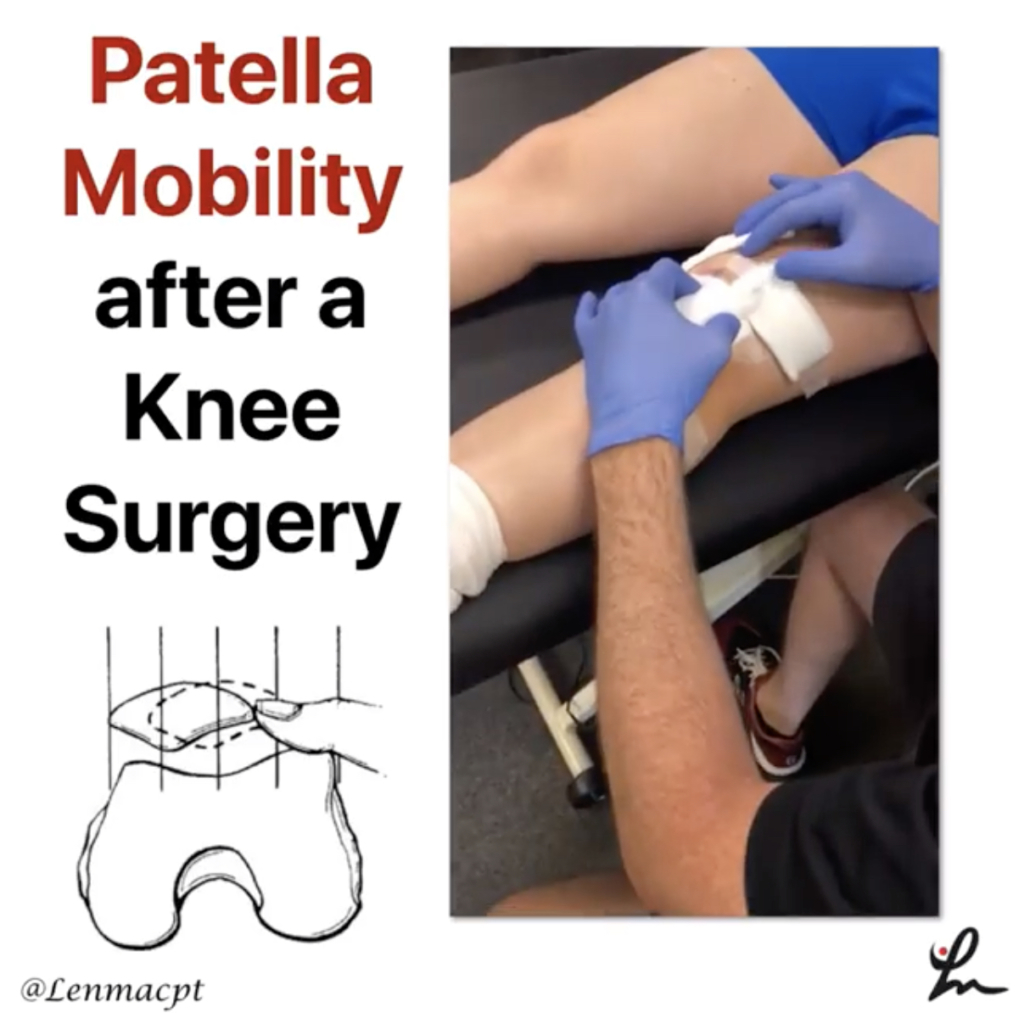
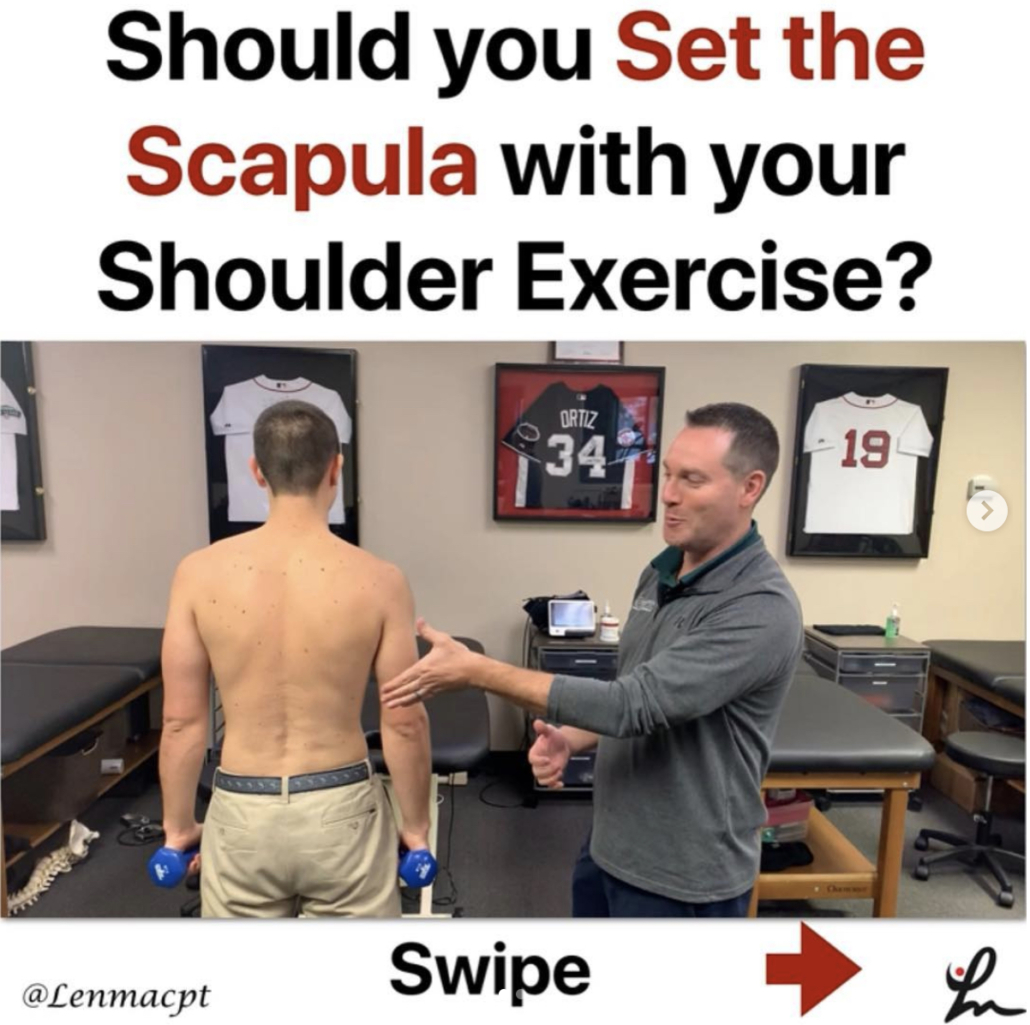
Normalize Patella Mobility
You must also normalize patella mobility, especially in a patella tendon autograft. It is critical to regain this mobility in order for the normal motions to occur in the knee and to restore normal arthrokinematics.
I don’t push things too quickly and think this sets the stage for the rest of the rehab. In my hands, slow and steady is the best approach. A spike in volume can slow things down.
When I say a spike in volume, it could simply be a long walk or an extra bike session. The patients are often feeling good and looking for some independence and normalcy. They want to push it and we need to let them know that an increase in swelling or pain can create an issue.
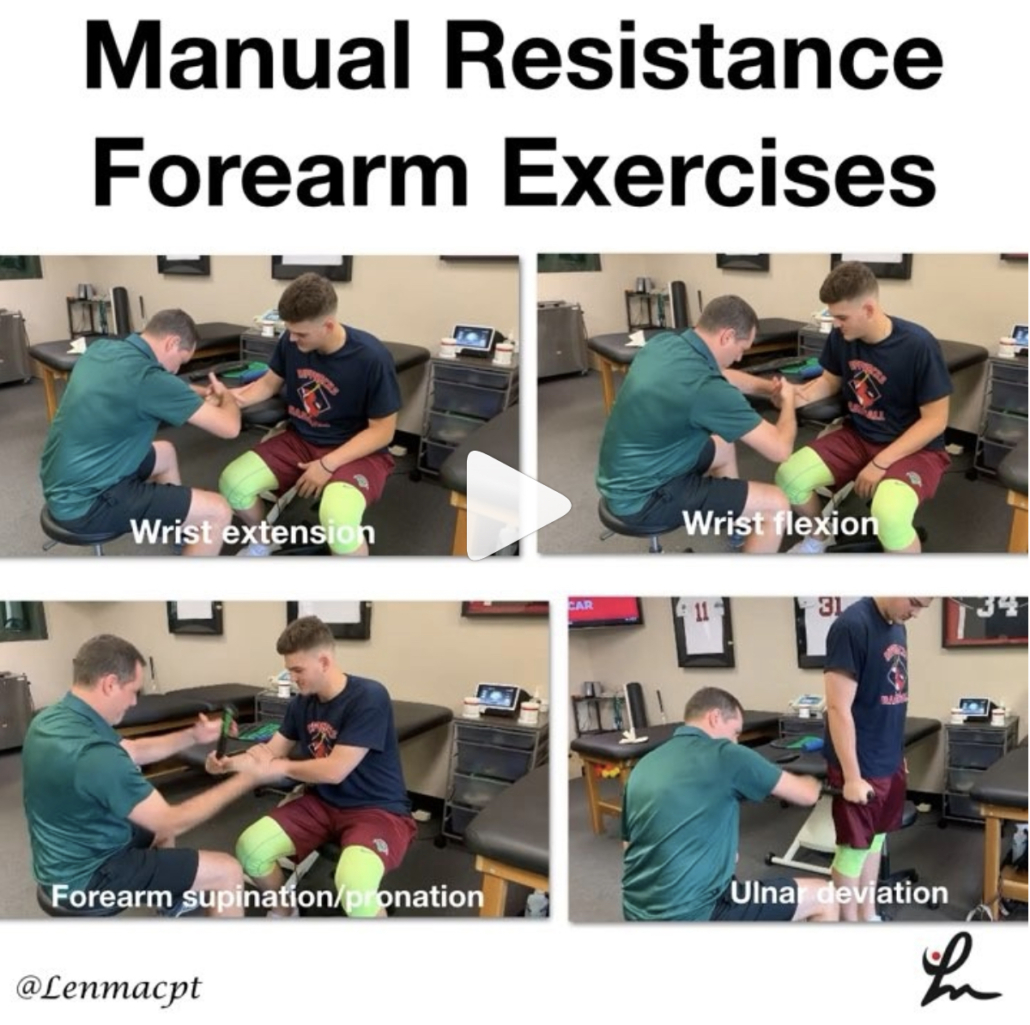
Strengthening
I tend to go pretty slow with this concept as well. I tend to stay conservative for 4-6 weeks and stay with mainly table exercises like leg raises and mini squats.
I do love to use electrical stimulation (I prefer the DJO Global Continuum 2 unit!) for the first 2 weeks then add blood flow restriction training to compliment the NMES.
Not sure the research backs up my thoughts besides this 2015 paper or this one from 2018 but it definitely shows promise and makes sense in my head.
I’ll stay with these particular exercises for 4-6 weeks to ensure that the knee is calming down and my exercise progressions are not causing more pain or swelling.
Let the ACL rehab fun begin
If you’ve made it this far, then the important concepts have been met. No really!
The first 6 weeks set the tone and it can only go up from here.
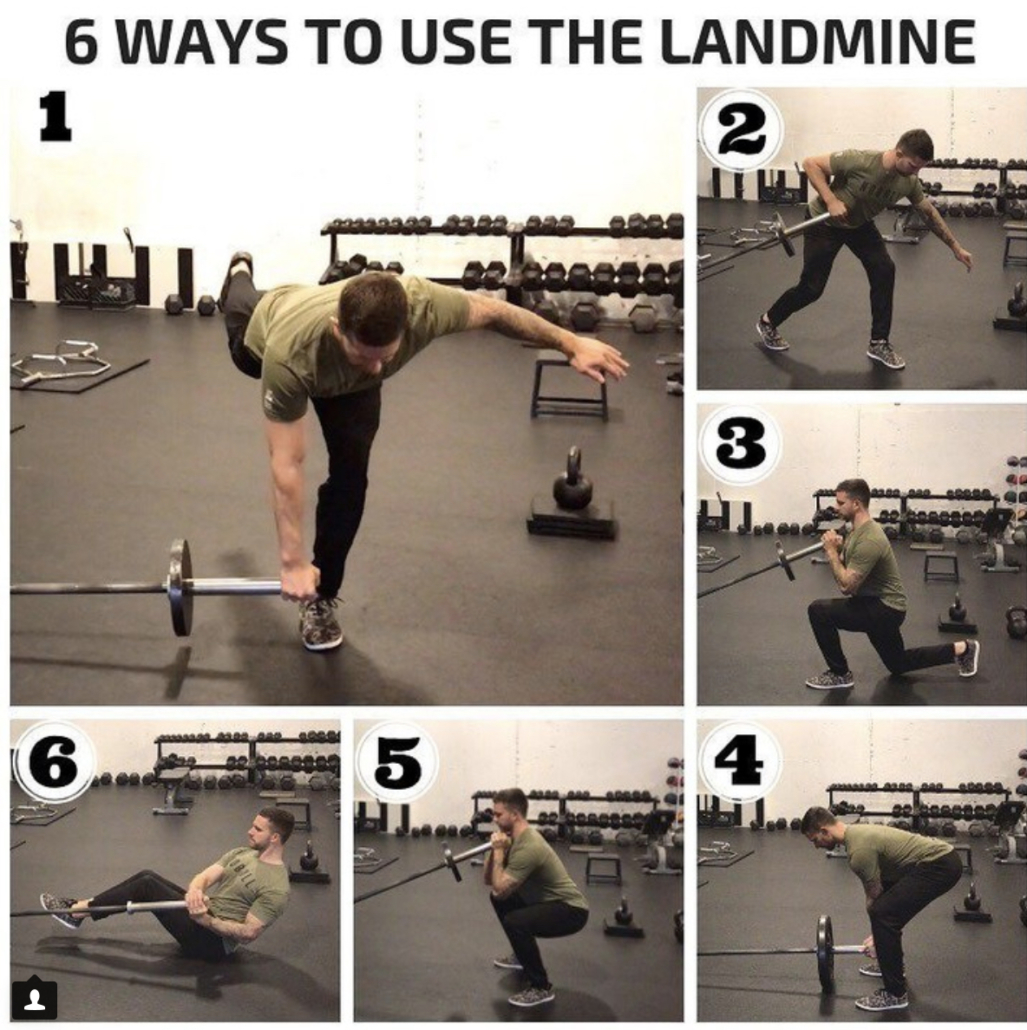
For my patients, I basically turn into a strength coach and progress them based on muscle capacity and progress their programs based on movements and muscle groups.
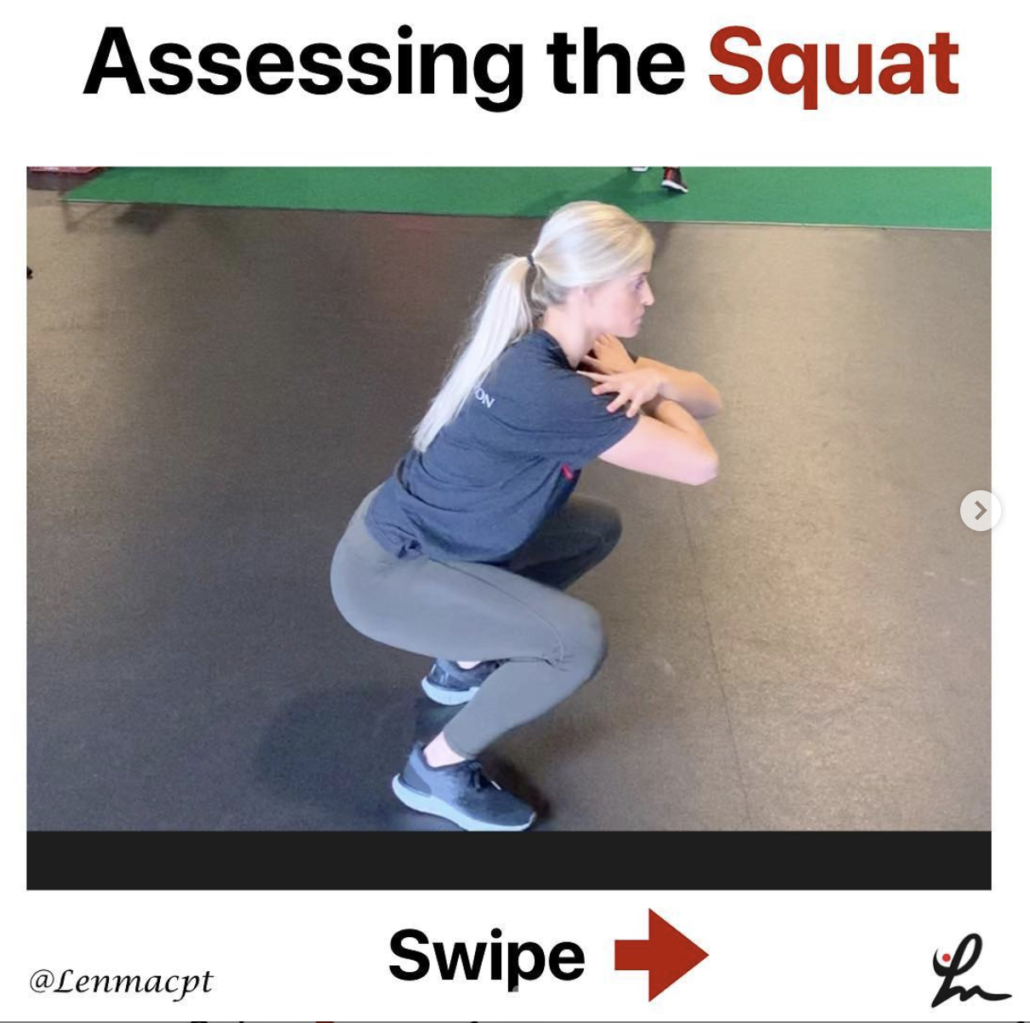
I like to really hammer single leg work early but only after I’ve given them a good bout of 2-legged work to establish a base of movement.
Some do it the other way but I want to build confidence with 2-legged squats and/or deadlifts to reinforce a movement then use single leg work to take it to the next level.
When to run after an ACL
As I’ve gotten older in my career, I’ve gotten slower with my progressions. I typically don’t like to start running until at least 4 months after surgery and that’s if their quadriceps muscle is strong enough.
I look to this paper that shows a quadriceps strength to bodyweight ratio (QS/BW) of 1.45 Nm/Kg as a rough estimate to initiate running.
Some may argue that this paper only considers ACL patients that utilized a hamstring autograft and that’s a fair argument. But there’s limited information out there and I wanted something more objective.
So, until they can establish a good quadriceps contraction and their ROM/gait are normalized, I will hold off running.
ACL rehab is mainly about strengthening
The cat’s out of the bag…don’t tell anyone!
It’s pretty simple, once you get through that 6 week interval that we talked about earlier.
If you’re not proficient in this, find someone who is in your area.
Otherwise, program using simple strength training principles that incorporate power, velocity, full ROM and tempo. Work on their aerobic capacity while building strength, power and endurance.
I could write another full blog post on this but we touch upon these concepts in our all online knee course.
Hope this helps!