The Week in Research Review, etc 10-8-18
Hey all, the Week in Research Review, etc 10-8-18 has some great articles that really got some good discussion going. I highly recommend reading each post and chiming in. Looking forward to the new comments and discussions!
- PT Continuity of care
- Fatigue effects on ACL tears
- Measuring IR in a baseball pitcher
- Lever sign to diagnose an ACL tear
- Immediate or delayed ROM after a rotator cuff repair
Longitudinal continuity of care is associated with high patient satisfaction with physical therapy. Beattie et al Phys Ther 2005.
I saw a FB post the other day and it reminded me of a study that I had seen about continuity of care and physical therapy.⠀
This study looked to provide ‘preliminary information regarding the association between longitudinal continuity and reports of patient satisfaction with physical therapy outpatient care.’
What they showed was “Subjects who received their entire course of outpatient physical therapy from only 1 provider were approximately 3x more likely to report complete satisfaction with care than those who received care from more than 1 provider.”
All too often, I hear my current clients talk about their past PT sessions and often complain about seeing a tech/aide or a different PT for each session.
I always thought that was such a wrong concept for the client. Throughout my career, I have strived to connect with each client in an attempt to help them overcome an injury.
We did this at @championsportsm in Birmingham and we do it now in Boston at @championptp.
It is such a game changer for the client when they have complete faith in their treatment, can connect with their PT and their PT can connect with them.
Just my little soapbox rant on continuity of care. Are you able to maintain a good continuity of care with your patients or are you constantly sharing and/or just doing evals?
Tag a friend or colleague who may benefit from this post…thanks!⠀
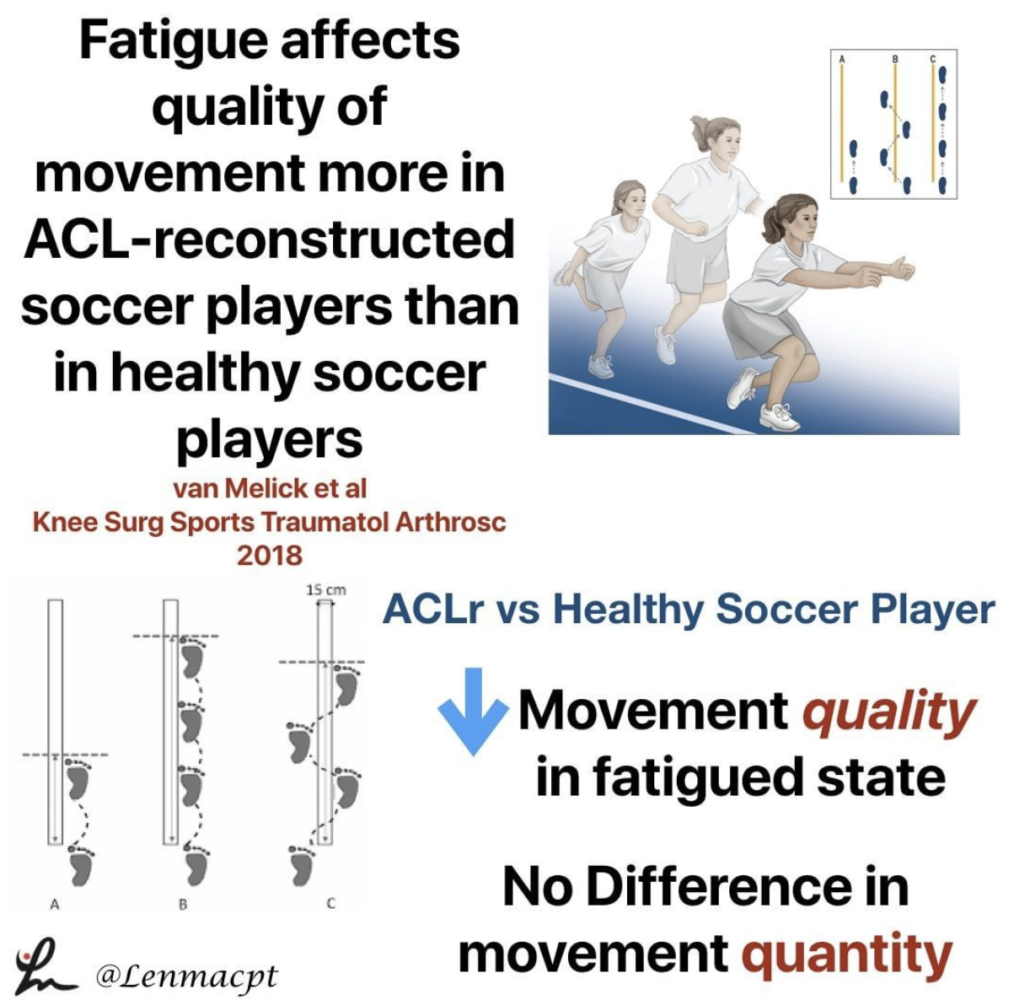
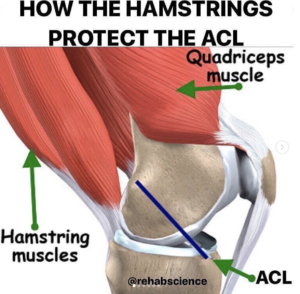
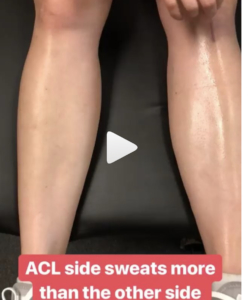
Fatigue affects quality of movement more in ACL-reconstructed soccer players than in healthy soccer players. van Melick et al Knee Surgery, Sports Traumatology, Arthroscopy 2018.
This study looked at the influence of neuromuscular fatigue on both movement quantity and quality in fully-rehabilitated soccer players after ACLR and to compare them with healthy soccer players.
They showed ACL-reconstructed soccer players had a significantly decreased performance when comparing the non-fatigued with the fatigued state.
For movement quantity, they used a single-leg vertical jump, a single-leg hop for distance, and a single-leg side hop.
For movement quality, they used a double-leg countermovement jump with frontal and sagittal plane video analyses. The Borg Rating of Perceived Exertion (RPE) scale was used to measure fatigue after a soccer-specific field training session. In addition to soccer-specific drills, exercises focussing on speed, stability, and coordination were included in this session.
Seems like a pretty neat study that may help to show us that the fatigued state influences quality of movements and not the quantity of movements. I know Tim Hewett has said that there’s no evidence that fatigue influences ACL tears but maybe this study is the 1st step.
Do you agree with this study? Anecdotally it makes sense but there’s little evidence to support the notions.⠀
⠀
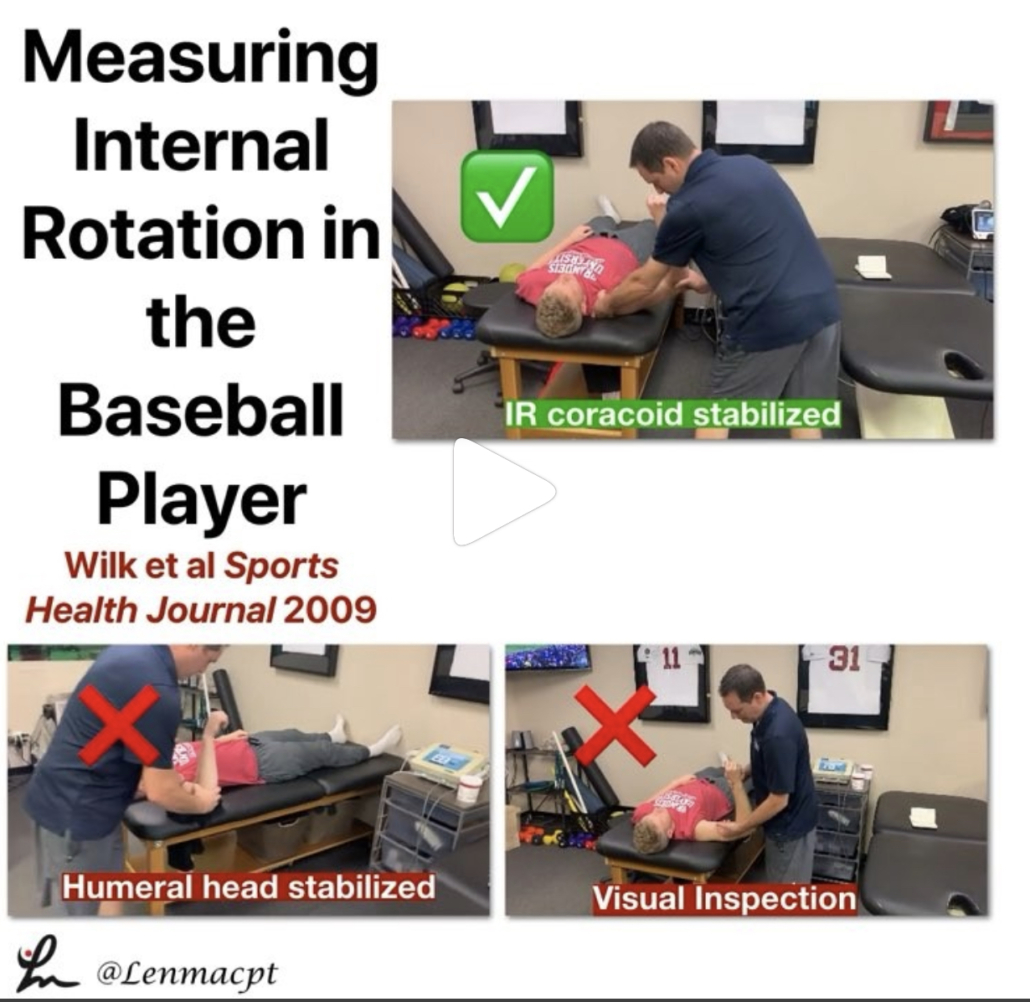
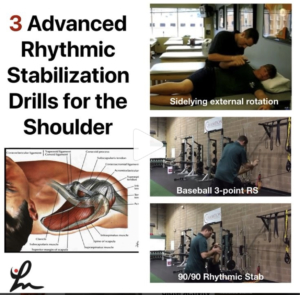
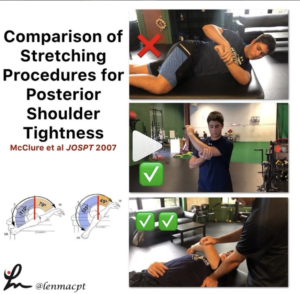
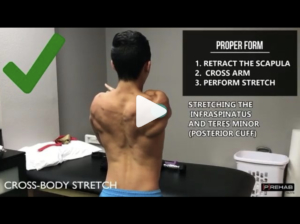
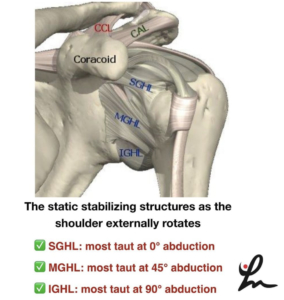
Measuring internal rotation in the baseball player
If you treat baseball pitchers, then you should have a good understanding of how to measure internal rotation of the shoulder joint.
Measuring internal rotation of the shoulder is one part of the equation when obtaining total rotational range of motion (TROM). Total rotational range motion is the sum of external rotation plus internal rotation. I use this equation weekly, if not daily when assessing my baseball players’ shoulders.
In a study in 2009 Sports Health Journal titled “Glenohumeral internal rotation measurements differ depending on stabilization techniques”, we looked at 3 different ways to measure IR. We determined that the scapula stabilized method had the best intra-rater reliability.
We also felt this was the best method to measure pure internal rotation of the glenohumeral joint.
Is this how you measure IR in your baseball pitchers? Do you consider TROM when making treatment recommendations?
Let’s talk it out and discuss the concept of TROM and how to measure it.
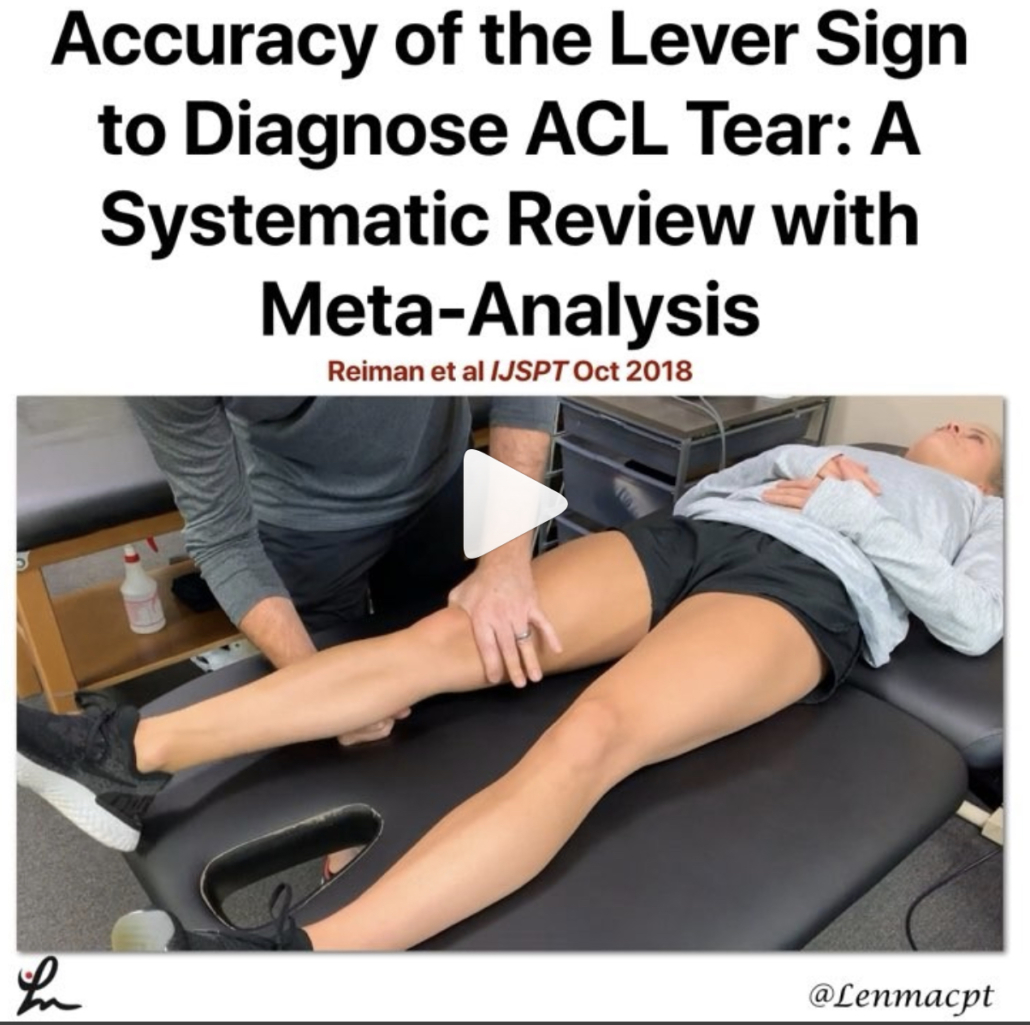
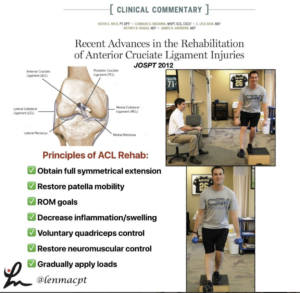
Accuracy of the Lever Sign to Diagnose Anterior Cruciate Ligament Tear: A Systematic Review with Meta-Analysis. Reiman et al IJSPT Oct 2018
This study was a systematic review with meta-analysis that hoped to summarize the diagnostic accuracy of the Lever sign for use during assessment of the knee for an ACL tear.
They showed that based on limited evidence, the Lever sign can moderately change posttest probability to rule in an ACL tear.
I’m a bit surprised by the limited studies because I’ve had a more difficult time getting consistent results compared to the Lachmans test (definitely my go-to!).
For those not familiar with the Lever test, it was 1st published by Dr Lelli in Knee Surg Sports Traumatol Arthrosc. 2016.
From the review, ‘The test requires the evaluator to place their fist under the calf muscle to create a “fulcrum” extending the knee while applying a moderate downward force to the distal part of the femur.
In an intact knee, the ACL completes a lever mechanism, making the heel rise in response to the force applied to the femur. In an ACL-deficient knee, the heel does not rise indicating a positive Lever sign.’ I have personally struggled to get consistent accuracy using the test. My results have been inconsistent with MRI results.
I’ve also struggled to do the test on a plinth that has padding and often have patients lie on a firm surface like the floor (which is very weird) in order to get a better test result.
Some people are freaked out by the method of the test. The clinician has to apply force to the knee in order to create the fulcrum. Many have not liked that force applied to the knee.
In general, this is not my go-to for a suspicious ACL tear. I have tried and still ty to use it but my results have been less than stellar.
Have you used this test for an ACL tear? Do you like it to supplement your Lachmans?
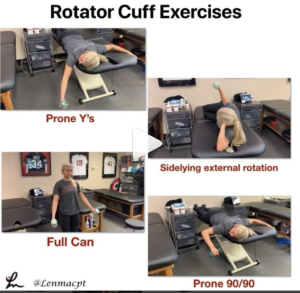
Should we delay PROM after a rotator cuff repair?
It seems as if we’re all over the place, which usually says the research is not cut and dry. There are so many factors that are considered when trying to figure out the best time to initiate motion.
I’m not talking active ROM or strengthening…I”m talking about passive ROM by a rehab specialist like a #PT, #OTor #ATC. Obviously, the docs weigh in heavily with this decision. I feel as if patients are restricted for the wrong reasons and could potentially begin PT earlier than we often see.
This is going to be a beast of a blog post and may alter my thinking, we’ll see.
As of now, I fully embrace immediate PROM for most post-op rotator cuff repairs, including Large and Massive repairs.
For revisions, we may need to think it through but I still feel as if most benefit from early PROM. We did it for years and with very good results during my time in Birmingham but feel as if maybe the pendulum is swinging in the conservative direction (for the wrong reasons).
What do you guys do? Do you have any input with your docs and can influence their rehab decisions? Let’s talk it out now and get prepped for my blog release in the coming days, weeks, months…whenever I can make it the best!⠀