Tag: baseball
-
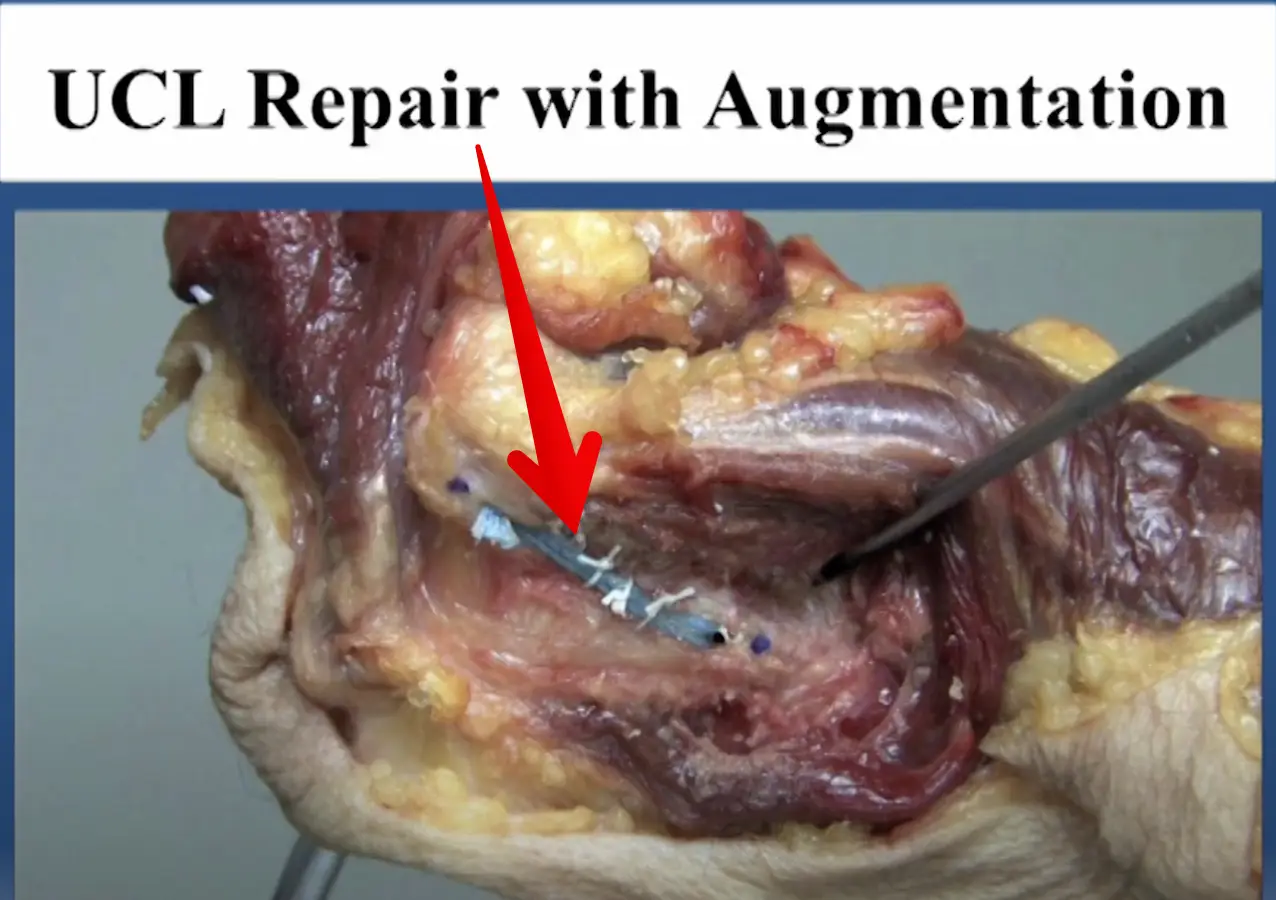
Diagnosed with an elbow UCL Tear- Reconstruction or Internal Brace surgery?
—
by
So, you’ve been diagnosed with a UCL tear in your elbow and your world has been turned upside down. Have no fear, many have been there before you and have done pretty well. But now, there’s a new option for elbow surgery and you’re not sure if it’s right for you. I hope this post…
-
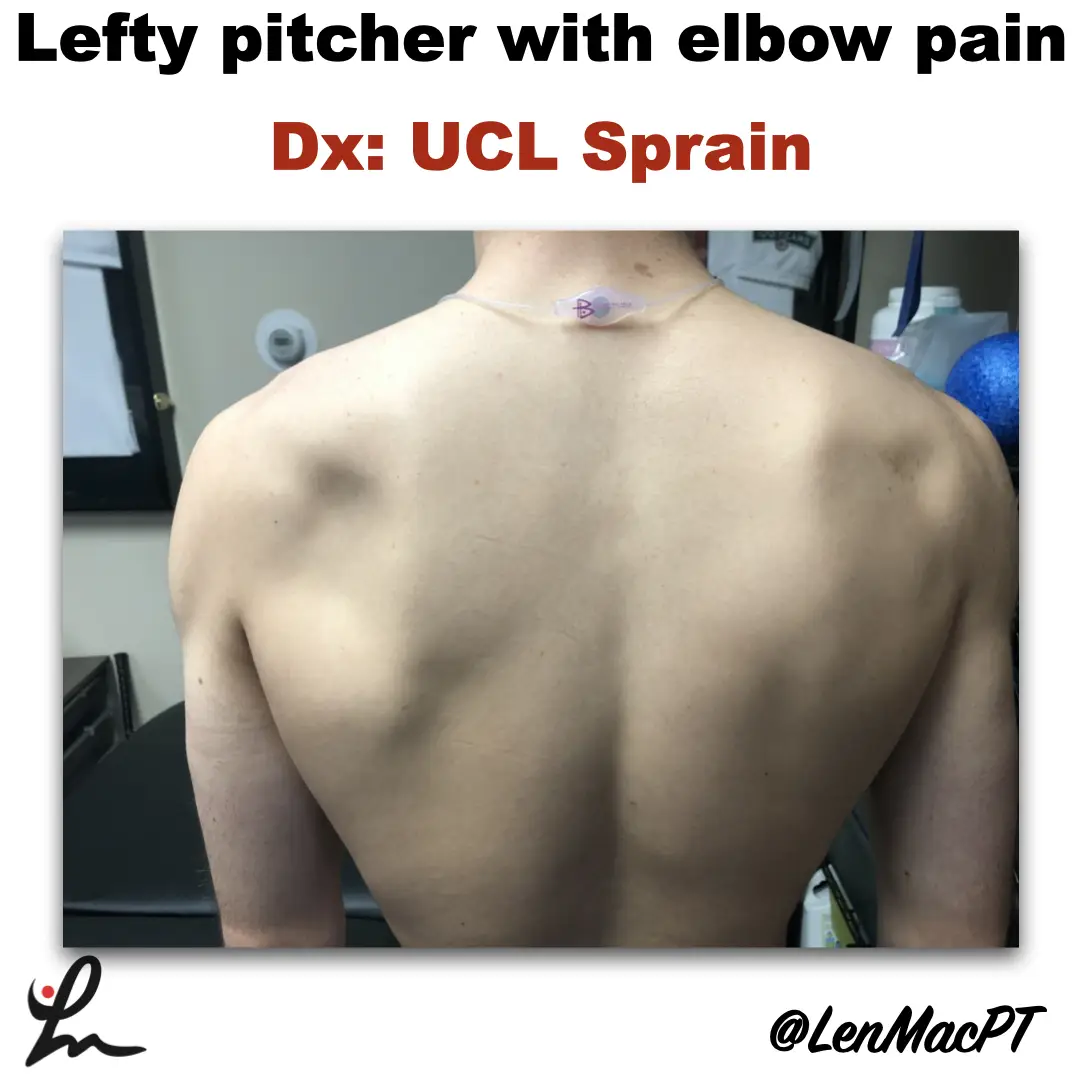
Infraspinatus atrophy in a baseball pitcher with a UCL sprain
—
by
Infraspinatus atrophy due to a spinoglenoid notch cyst This was an incidental finding of mine in a collegiate baseball pitcher. He presented with a UCL sprain during his senior year and was struggling. He came in looking to salvage his senior year and attempt to pitch at some point. UCL surgery would’ve been warranted if…
-
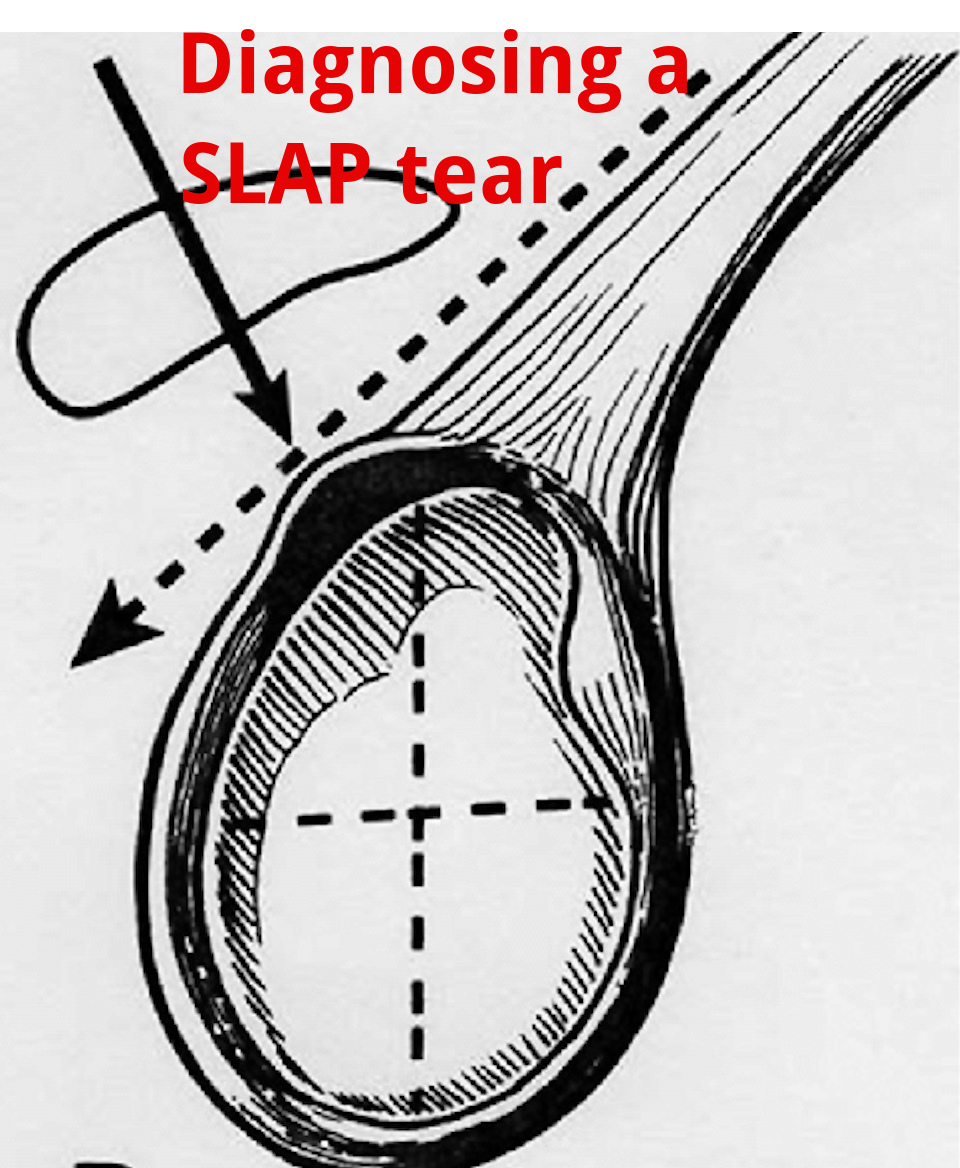
An Update on Diagnosing SLAP tears
—
by
Diagnosing a SLAP tear is not easy We hear a lot about trying to diagnose shoulder pain and to be as specific as possible. It’s often difficult to differentiate SLAP (superior labrum anterior to posterior) tears from other soft tissue injuries of the shoulder. For a review of the different types of SLAP tears, check…
-
The Week in Research Review, etc 11-19-18
—
by
Great ‘Week in Research Review, etc 11-19-18’ that I hope you find helpful to your practice. I’ve always touted the importance of the subjective portion of the exam so I wanted to share a slide from a recent talk I gave to a group in Canandaigua, NY. Obviously, the squat is a fundamental movement and…
-
The Week in Research Review, etc 11-12-18
—
by
This week in research review for 11-12-18 we focused a bit more on assessment and also dabbled in some basic treatment strategies for the back and shoulder. Check out the topics below and like them or comment on Instagram to keep the conversation going…thanks all! A quick fix for a sore low back? Knee…
-
The Week in Research Review, etc 11-5-18
—
by
in ACL, DPTstudent, emg, exercise, general, hip, knee, Physical Therapy, rehabilitation, Research, rotator cuff, ShoulderThe Week in Research Review, etc 11-5-18 was filled with more informative and eye-opening posts! Lots of visually stimulating posts to help clarify what exactly is going on in the hip joint with PROM. Another post that shows the suction effect from an intact hip labrum… amongst other great posts. Just some great stuff..hope you…
-
The Week in Research Review, etc 10-22-18
—
by
That was a milestone week as my Instagram account finally hit 10k followers, whatever that means! I’ve really been pushing a daily post to help other rehab professionals better simplify the research. One milestone hit but I still want to keep publishing good quality research reviews. The Week in Research Review, etc 10-22-18 included: Do baseball Pitchers…
-
The Week in Research Review, etc 10-8-18
—
by
in ACL, baseball, DPTstudent, elbow, general, hip, knee, Physical Therapy, rehabilitation, Research, rotator cuff, ShoulderHey all, the Week in Research Review, etc 10-8-18 has some great articles that really got some good discussion going. I highly recommend reading each post and chiming in. Looking forward to the new comments and discussions! PT Continuity of care Fatigue effects on ACL tears Measuring IR in a baseball pitcher Lever sign to…
-
The Week in Research Review, etc 10-1-18
—
by
Another week of some great discussions and learning opportunities. The Week in Research Review included: Risk Factors for Patellofemoral pain Shoulder ROM and elbow injuries Rotator Cuff Exercises Eccentric or Concentric exercise for Tendinopathy Hamstrings Protect the ACL Stretching the Shoulder in the Overhead Athlete Share with your friends and have them subscribe to the weekly newsletter!…
