Category: emg
-
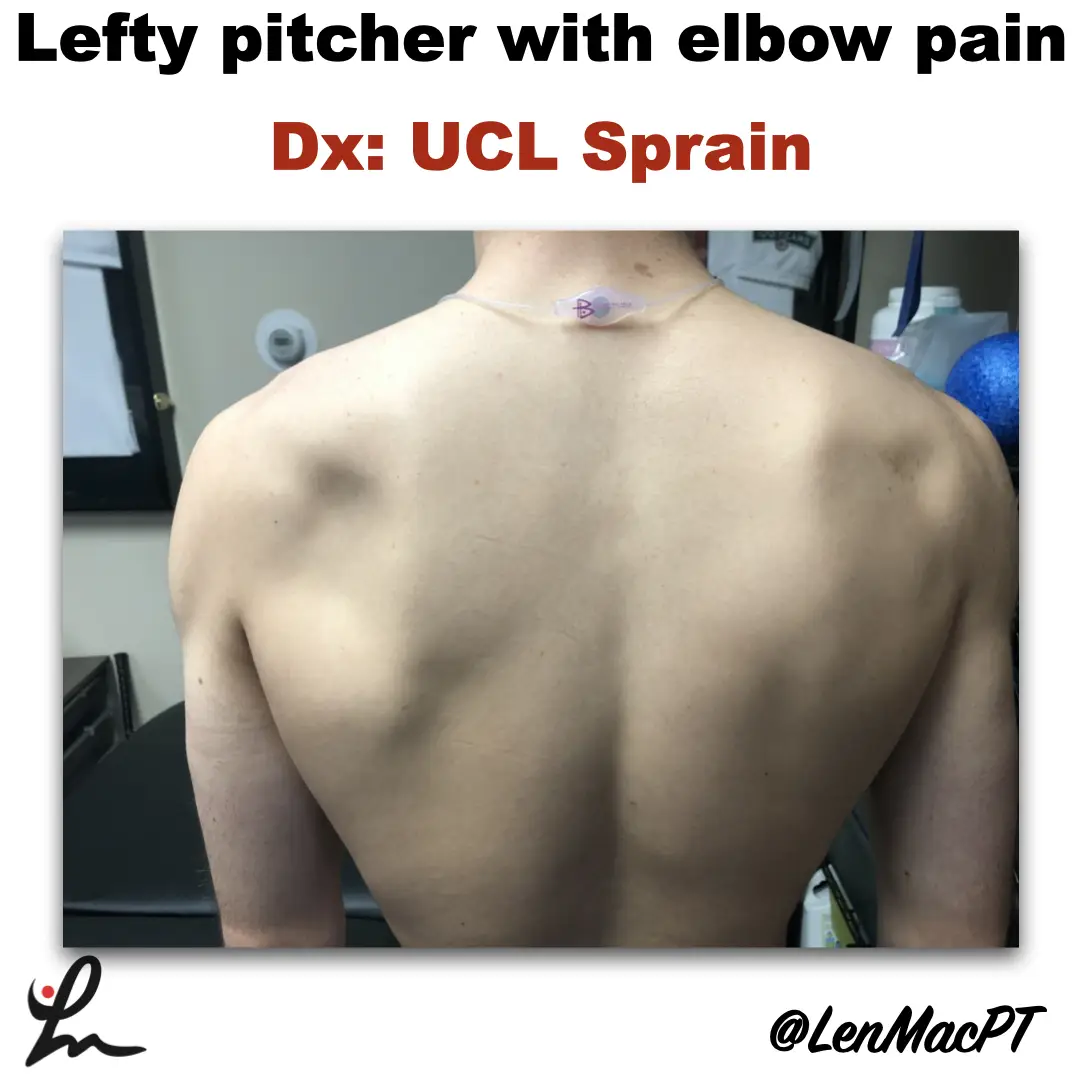
Infraspinatus atrophy in a baseball pitcher with a UCL sprain
—
by
Infraspinatus atrophy due to a spinoglenoid notch cyst This was an incidental finding of mine in a collegiate baseball pitcher. He presented with a UCL sprain during his senior year and was struggling. He came in looking to salvage his senior year and attempt to pitch at some point. UCL surgery would’ve been warranted if…
-
Is Early Physical Therapy Safe After a Rotator Cuff Repair?
—
by
Physical therapy is vital after a rotator cuff repair and continues to be common in an outpatient setting. Unfortunately, there’s no true consensus on when to actually begin PT. Is early physical therapy safe after a rotator cuff repair or should we delay PT to protect the healing tendons? Let’s dive into this and see what the research…
-
The Week in Research Review, etc 12-17-18
—
by
Not a lot this week…sorry folks. Focusing a bit more on other projects. The Week in Research Review, etc 12-10-18 included only 3 posts but they definitely made some waves. Especially my latest Instagram post on burn-out in the PT field. Check it out and chime in…it’s never too late to like a post and comment…
-
The Week in Research Review, etc 12-10-18
—
by
This week we’re still playing with formats and learning these Instagram changes. With that, in the week in research review 12-10-18, we discussed many topics that I wanted to share! Surgery vs Physical Therapy for Carpal Tunnel Syndrome View this post on Instagram A post shared by Lenny Macrina MSPT, SCS, CSCS (@lenmacpt) on Dec…
-
The Week in Research Review, etc 12-3-18
—
by
Hey everyone, The Week in Research Review, etc for this week has a new look, compliments of Instagram’s new algorithm. Hope the new format doesn’t throw you too big of a curveball (maybe you’ll like it better), so here goes… ACL Injury Rates Higher on Synthetic Turf than Natural Grass in the NFL Preventing…
-
The Week in Research Review, etc 11-5-18
—
by
in ACL, DPTstudent, emg, exercise, general, hip, knee, Physical Therapy, rehabilitation, Research, rotator cuff, ShoulderThe Week in Research Review, etc 11-5-18 was filled with more informative and eye-opening posts! Lots of visually stimulating posts to help clarify what exactly is going on in the hip joint with PROM. Another post that shows the suction effect from an intact hip labrum… amongst other great posts. Just some great stuff..hope you…
-
The Week in Research Review, etc 10-22-18
—
by
That was a milestone week as my Instagram account finally hit 10k followers, whatever that means! I’ve really been pushing a daily post to help other rehab professionals better simplify the research. One milestone hit but I still want to keep publishing good quality research reviews. The Week in Research Review, etc 10-22-18 included: Do baseball Pitchers…