The Week in Research Review, etc 11-12-18
This week in research review for 11-12-18 we focused a bit more on assessment and also dabbled in some basic treatment strategies for the back and shoulder. Check out the topics below and like them or comment on Instagram to keep the conversation going…thanks all!
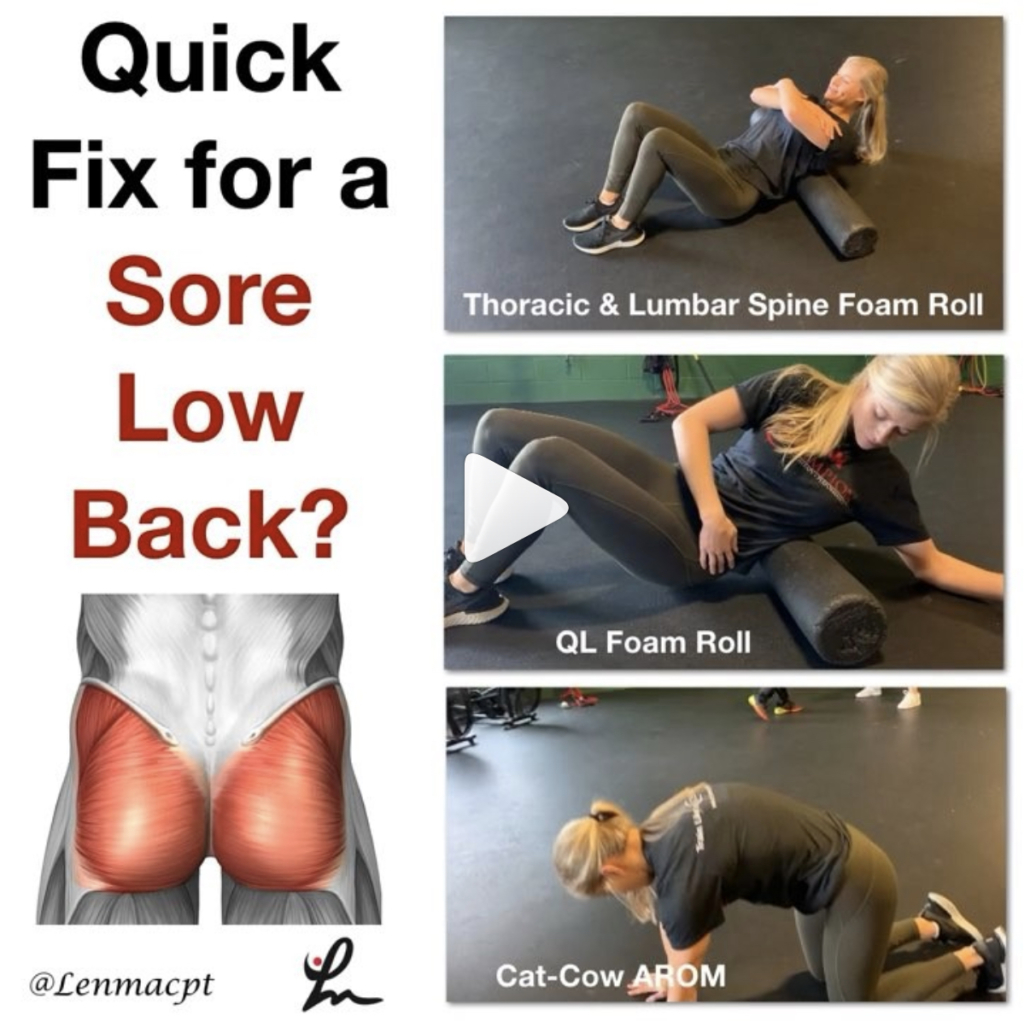
- A quick fix for a sore low back?
- Knee Fat Pad Testing and Diagnosis
- How to Assess the Elbow for a Tommy John (UCL) Sprain
- Lumbopelvic control on shoulder and elbow kinetics in elite baseball pitchers
- Full Can or Empty Can? – by @mikereinold
Looking for a quick fix for a sore low back?
I’m speaking from personal experiences when I post a few of the common exercises that have helped me tremendously in the past.
I’m not saying that this is all you have to do but I do think that new onset of low back soreness, you know that tightness that you feel on either side of your spine, can be somewhat alleviated with some foam rolling and active range of motion.
I would definitely include more focal strengthening of the core like deadbugs and bird dogs, squats, deadlifts (when they’re ready), etc.
But for the purpose of this post, I think some foam rolling and motion to the area can take the edge off of someone’s soreness and get them feeling a little better. That’s my goal for many and hopefully those small gins can add up to big gains in the long run!
Do you utilize these techniques as well? If you don’t, then I suggest that you try! They’ve helped me numerous times and continue to help me when my soreness gets a bit out of control.
Tag a friend who may want to check out this post…thanks!
Thanks @corrine_evelyn for the demos!
Knee Fat Pad Testing and Diagnosis
Here’s an excerpt from a previous blog post where I talked about anterior knee pain fat pad irritation. Link in bio!
Keep in mind, my differential diagnosis is all over the place at times. With knee pain you need to consider:
Meniscus (see my previous blog post)⠀
ITB
Osteochondral lesion
Patella tendonitis
Pes anserine bursitis
MPFL sprain
Hamstring strain
Plica syndrome
MCL/LCL
Tumor
Infrapatellar fat pad irritation can be functionally debilitating. I believe it presents itself pretty often in the clinic, more than most PT’s realize.
Use this test to see if it truly is a fat pad issue.
How to Assess the Elbow for a Tommy John (UCL) Sprain
In this excerpt from my YouTube channel, I discuss the tests that I use to help identify an elbow sprain, typically seen in the baseball players that I treat.
In the full video, I discuss:
✅Joint Palpation
✅Seated Milking Sign
✅Prone Valgus Test (maybe a new one for you!)
✅Supine end range External Rotation with Valgus Extension Overload (VEO)
I also wrote a blog post about this topic so hopefully you’ll go to my site and read a bit more about this.
If you treat baseball players of all ages, then you should know how to diagnose a UCL sprain.
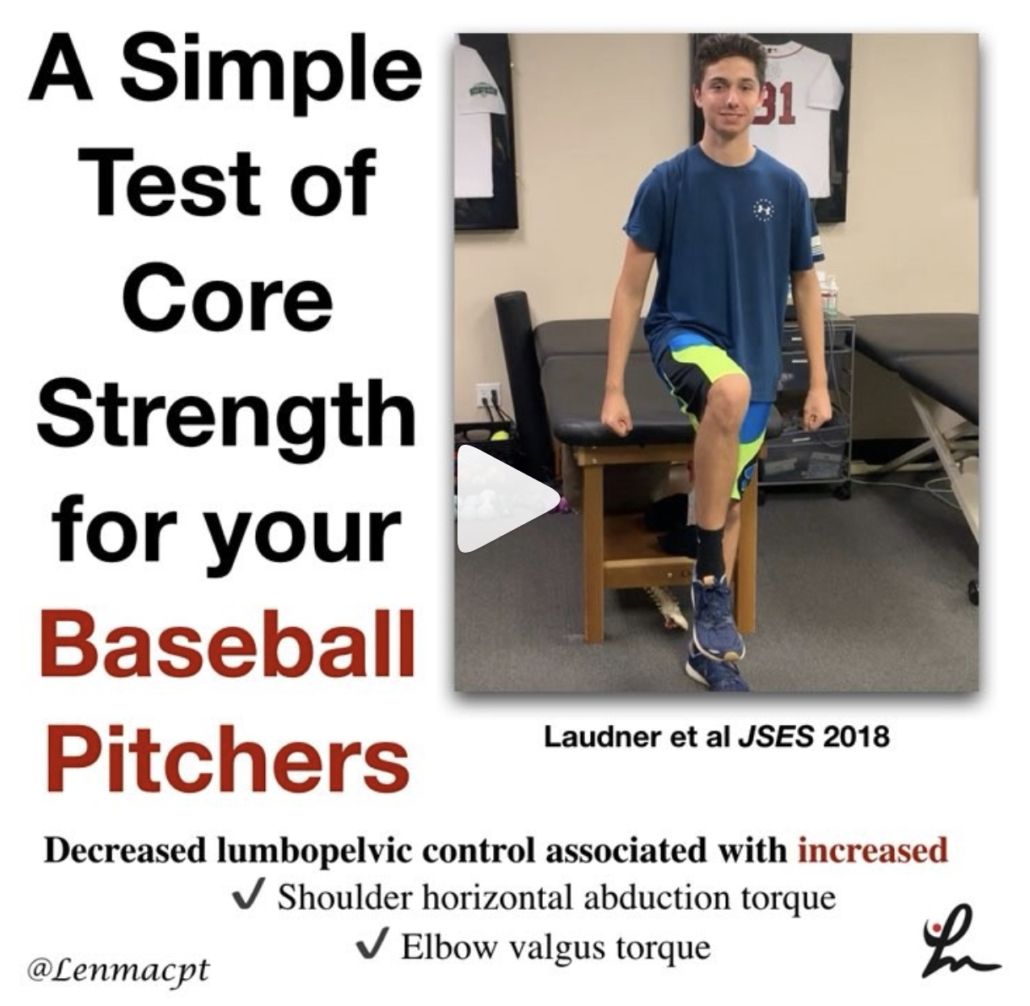
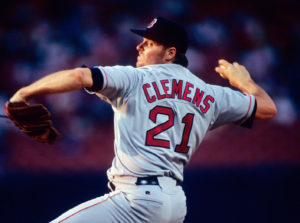
The influence of lumbopelvic control on shoulder and elbow kinetics in elite baseball pitchers
Laudner et al JSES 2018.
This study looked at 43 asymptomatic, #NCAA Division I and professional minor league baseball pitchers. They measured the bilateral amount of anterior-posterior lumbopelvic tilt during a single-leg stance trunk stability test.
The Level Belt Pro (Perfect Practice, Columbus, OH, USA) was used to assess anterior-posterior lumbopelvic control. The LevelBelt Pro consists of an iPod–based digital level secured to a belt using hook-and-loop fasteners.
This test has been used and studied previously by Chaudhari et al (JSCR 2011) and he showed that pitchers with less lumbopelvic control produced more walks and hits per inning than those with more control.
Also, pitchers with less lumbopelvic control have been shown to have an increased likelihood of spending more days on the disabled list than those with more control (Chaudhari et al AJSM 2014).
“The results of our study show that as lumbopelvic control of the drive leg decreases, shoulder horizontal abduction torque and elbow valgus torque increase.”
Have you tried this simple test? I will say that having the ability to detect millimeters of motion is clinically difficult.
It is good to see such a simple test utilized clinically can help aid in determining the need for more core/hip exercises for our pitchers. In all, I think it’s a safe bet to incorporate these exercises in all pitchers’ programs.
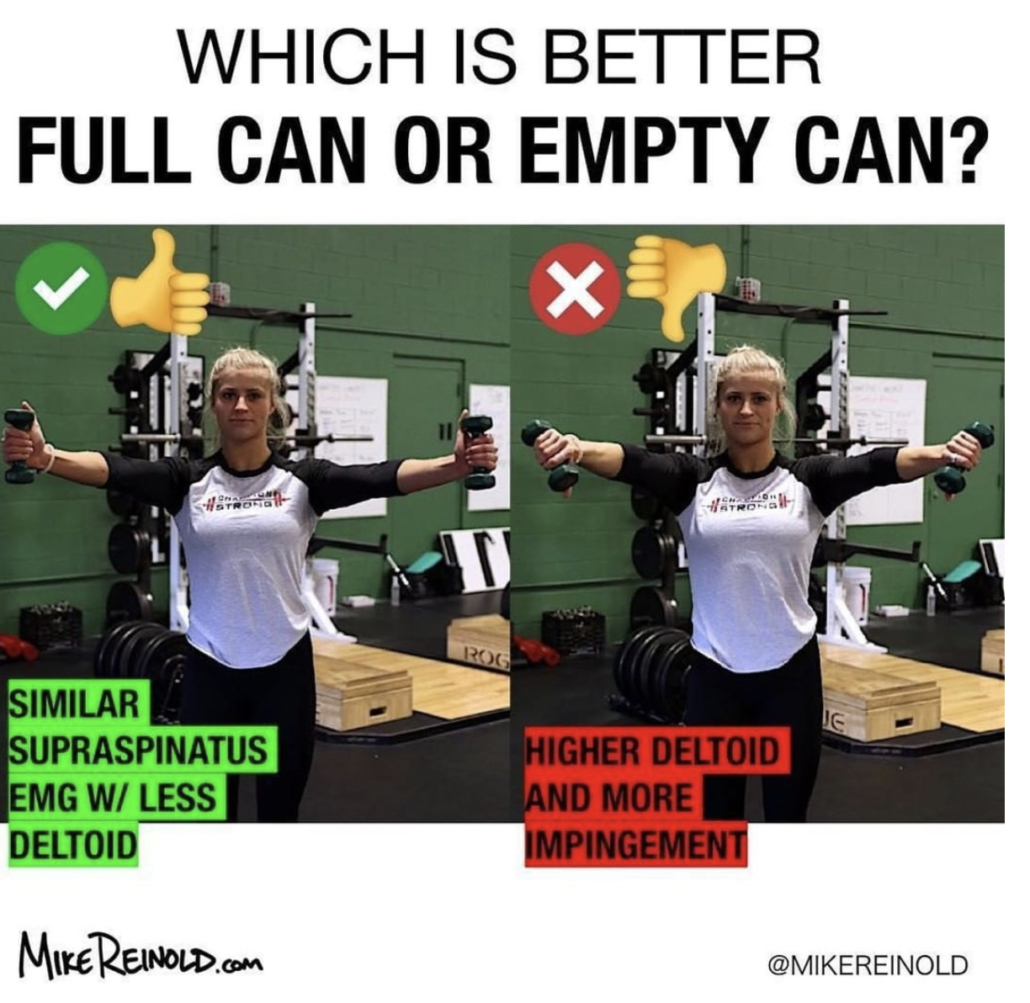
Full Can or Empty Can?
– by @mikereinold
Great Post by @mikereinold on which motion is BEST to isolate the supraspinatus during arm elevation. I know you can’t isolate the supraspinatus but numerous studies have (Kelly et al 1996, Reinold et al 2004) shown that the full can (or thumb up position) is better than the empty can position.
Check it out below! 👇🏼
Full Can or Empty Can? – by @mikereinold⠀⠀
-⠀⠀
🧠 WANT TO LEARN MORE FROM ME? Head to my website MikeReinold.com, link in bio.⠀⠀
-⠀⠀
I’m still surprised after all these years that I still see the empty can exercise kicking around. I analyzed these two movements many years ago in an article in JOSPT and showed that the full can exercise (thumbs up 👍) had similar EMG of the supraspinatus with lower levels of deltoid EMG, while the empty can (thumbs down 👎) had higher levels of deltoid EMG.
Why does this matter?
Well, think about it. If you are performing this exercise you probably are trying to strengthen the rotator cuff. And if you are weak and performing an exercise with more deltoid, the ratio of cuff to deltoid will be lower and you’ll have more potential for superior humeral head migration.
Plus, let’s be honest, the empty can just hurts… It’s also a provocative test, and I don’t like to use provocative tests as exercises. 😂😂😂⠀