The Week in Research Review, etc 8-19-18
We posted a lot of information this week to review so hopefully you were able to keep up with it all. If not, here’s a bunch of it from the week. Check it out and comment as you want. Lots of good information on:
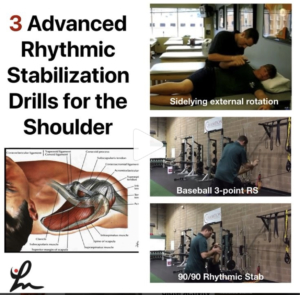
- Advanced Rhythmic Stabilization Drills
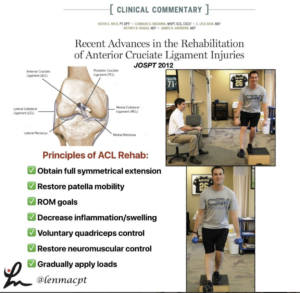
- Our ACL rehab paper from 2012
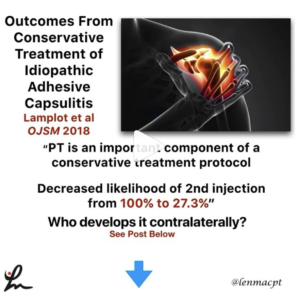
- PT usage for Frozen Shoulder
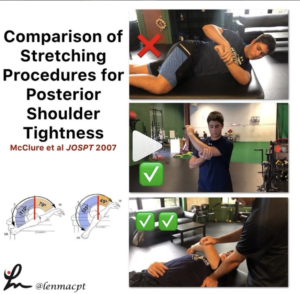
- Comparison of posterior shoulder stretching techniques
- Increased Sweating after an ACL surgery? Seems pretty common in the comments section
- @theprehabguys show how to do a posterior shoulder stretch
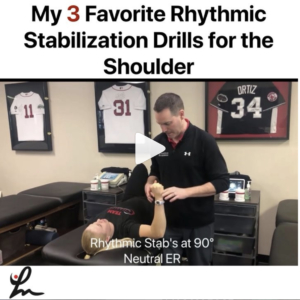
Advanced stabilization drills
These advanced stabilization drills are a great way to progress the patient once they’ve shown improved neuromuscular control with the basic drills from the other day.
I use these for most of my clients that need improved dynamic stability, especially those hypermobile athletes that play baseball, swim, or do gymnastics.
You can modify the speed and amount of force that I give during the drill based on how they are responding that day and how they have progressed overall. You can also increase the time of the drill to bring in an endurance component, as well.
The goal is to use these to prep the shoulder for higher level activities such as plyometrics, throwing, etc.
I want the shoulder joint to be as strong as possible. And most importantly, I want the client to perceive that their shoulder is stronger so that they are more confident!
Do you use these rhythmic stabilization drills with your patients?
Tag a friend who may benefit from these drills and try them on your patients the next time they’re ready to progress their dynamic stability drills!
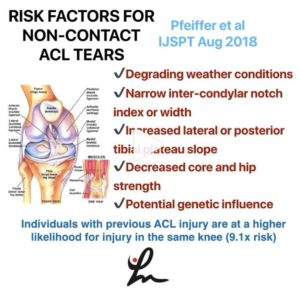
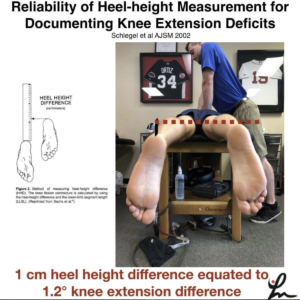
Recent advances in the rehabilitation of anterior cruciate ligament injuries. @wilk_kevin et al JOSPT 2012 @drlylecain @dugasmd1
We wrote this paper in JOSPT to help clinicians better understand the rehab involved after their patient undergoes an ACL reconstruction.
The paper discussed the principles of ACL rehab, including:
✅obtaining full symmetrical extension
✅restoring patella mobility
✅ROM goals
✅Decrease inflammation/swelling
✅voluntary quadriceps control
✅restore neuromuscular control
✅Gradually apply loads
We also discuss special rehab implications for:
✅The Female Athlete
✅Concomitant injuries (MCL, meniscus, LCL, cartilage lesions)
✅Implications of Graft type
Our Accelerated ACL-PTG protocol is included to help guide the rehab process and give the rehab specialist some goals to achieve.
Again, a protocol is just a guide and by no means meant to place aggressive limitations on a patient.
Hope this paper helps you to better understand ACL rehab. Tag a friend or colleague who may benefit from this post.
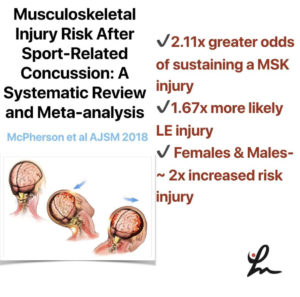
Outcomes From Conservative Treatment of Shoulder Idiopathic Adhesive Capsulitis and Factors Associated With Developing Contralateral Disease Lamplot et al 2018 OJSM 2018
A minimum 2-year follow-up of patients diagnosed with idiopathic adhesive capsulitis.
They were treated with a single intra-articular glenohumeral injection of local anesthetic and corticosteroid as well as 4 weeks of supervised PT.
Physical therapy reduced the use of a second injection as part of treatment. Contralateral disease was more likely in patients with diabetes and those younger than 50 years.
PT is an important component of a conservative treatment protocol, as PT decreased the likelihood of receiving a second injection from 100% to 27.3%.
In my opinion, a cortisone injection + PT is the best treatment ‘cocktail’ for someone with frozen shoulder, particularly in the freezing phase.
Do you guys agree? Let’s discuss this very debilitating pathology. Tag a friend who may want to discuss this further.
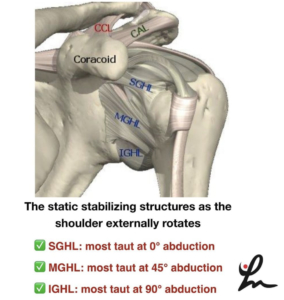
A Randomized Controlled Comparison of Stretching Procedures for Posterior Shoulder Tightness McClure et al JOSPT 2007
This study looked to compare changes in shoulder internal rotation range of motion (ROM), for 2 stretching exercises, the “cross-body stretch” and the “sleeper stretch,” in individuals with posterior shoulder tightness.
From their results, “The improvements in IR ROM for the subjects in the ✅cross-body stretch group (mean ± SD, 20.0° ± 12.9°) were significantly greater than for the subjects in the control group (5.9° ± 9.4°, P = .009). The gains in the ❌sleeper stretch group (12.4° ± 10.4°) were not significant compared to those of the control group (P = .586) and those of the cross-body stretch group (P = .148).”
Just be aware of the large standard deviations and low number of subjects…plus the subjects were all asymptomatic.
With that, I still believe clinically that the cross-body stretch is one of the better stretches for the shoulder. I have gotten away from the sleeper stretch because I don’t believe the risk/reward presents favorably.
✅✅I personally prefer the supine horizontal adduction stretch with the scapula stabilized. I feel like this best isolates the posterior soft tissue (mainly muscle, in my opinion) and that’s my target tissue.
Do you use the sleeper stretch with your patients or do you prefer the cross-body stretch?
Comment below and let’s talk about it. Also, tag a friend who may benefit from this post…thanks!
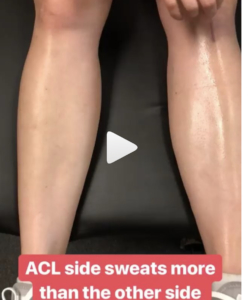
Sweating Leg after an #ACL
Had this in my story and posted to Twitter and got some pretty good discussion going. Is this some altered autonomic nervous system response after #ACLsurgery? I’ve seen it a bunch, where the area inferior to the incision sweats significantly more than the contralateral leg. Anyone else see this phenomenon and have an opinion? Have had people say that maybe it was compartment syndrome or CRPS but it happens with many many ACL patients so it seems very normal. What do you think? #ACL #ACLrehab
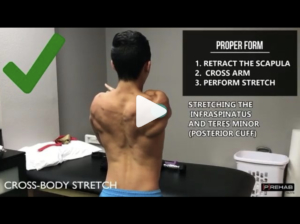
Horizontal Adduction Stretching
Perfect timing by @theprehabguys with their horizontal adduction post from the other day. Blends perfectly with the McClure 2007 et al study I posted the other day that showed horizontal adduction is the best way to obtain internal rotation mobility at the shoulder. I often tell people to wedge their lateral scapula against a wall to help stabilize but this way may also benefit them. Check out their post below!⠀
👇🏻⠀
Are You Performing The Arm Across Body Stretch Correctly⁉️⠀
[How to Stretch Your Posterior Cuff]
A tight posterior cuff is associated with a handful of shoulder dysfunctions like subacrominal impingement syndrome, posterior impingement, anterior instability, etc. And thus, ⬇️ tone/increasing extensibility of the posterior cuff is part of the treatment protocol for many with shoulder pain. The cross-body stretch is a fantastic way to target the posterior cuff but far too often it is done INCORRECTLY.
‼️In order to effectively stretch the posterior cuff, you need to keep your SCAPULA STABILIZED ie your scapula CANNOT MOVE!‼️
❌If you pull your arm across your body and your scapula comes with it into horizontal abduction, the only stretch your getting is of your mid-scapular muscles like your rhomboids or traps. Furthermore, in this position there’s more of a distraction force on the glenohumeral joint than a true stretch of the posterior cuff – aka not as specific as it can be.
✅First pull your shoulder blades back. This will keep your scapula in a retracted position. Only WHILE MAINTAINING THE POSITION OF YOUR SHOULDER BLADES BACK can you effectively target the posterior cuff. Pay attention to WHERE you feel the stretch, as you should feel a “deep stretch” in the back of your shoulder in the highlighted area on the video. If you feel a stretch or anything else not in the back of the shoulder, you’re either doing the stretch incorrectly or abutting other structures in your shoulder due to pathology (ie don’t do the stretch anymore and seek out a physio if you’re in pain).
Try it out and let us know how it feels! Tag a friend who NEEDS this stretch! #shoulderstretch #posteriorcuff#posteriorcapsule