Tag: surgery
-

Simplifying ACL Rehab
—
by
ACL surgery continues to be a huge focus in the literature and in our outpatient rehabilitation settings. Numerous studies focus on return to play guidelines and retear rates. Social media is all over the place, most times. Let’s try to make things simple and set the stage early. Paralysis by Analysis- What ACL tests are…
-

Risk Factors for Recurrent Instability After a Bankart Repair Surgery
—
by
Recurrent instability after a Bankart repair surgery is unfortunately very common. This paper looks to highlight the most common risk factors associated with recurrent instability. I thnk it’s valuable to understand these various risk factors so you can better educate your patients. It may also help clinicians be mindful of the people that may need…
-

ACL Volume Changes over a Women’s Soccer Season
I’m a bit interested, confused and looking to seek more on this open access paper that just came out in March of 2019 looking at the effects of season-long participation on ACL volume in female intercollegiate soccer athletes. The title of the paper is: “Effects of season-long participation on ACL volume in female intercollegiate soccer…
-
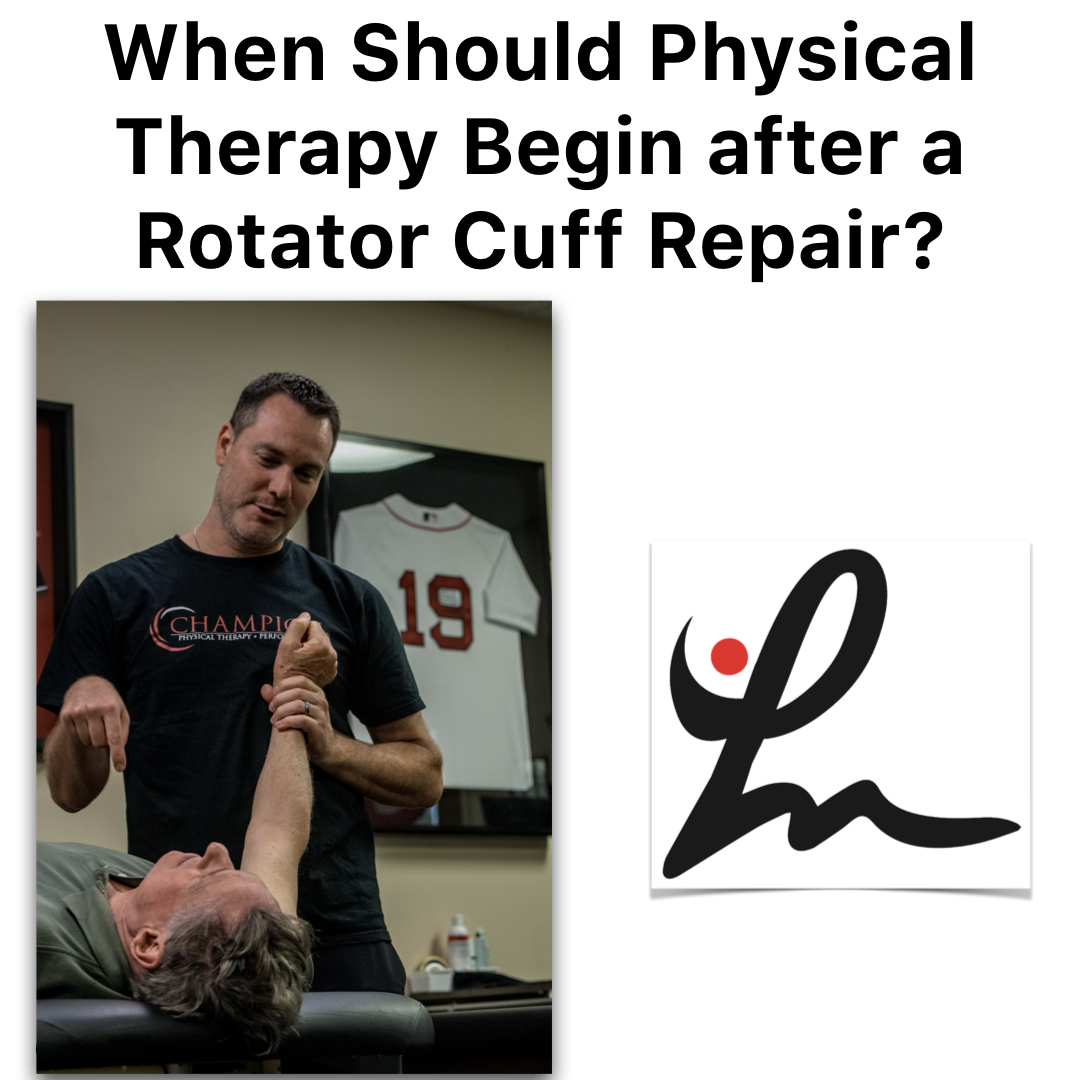
Is Early Physical Therapy Safe After a Rotator Cuff Repair?
—
by
Physical therapy is vital after a rotator cuff repair and continues to be common in an outpatient setting. Unfortunately, there’s no true consensus on when to actually begin PT. Is early physical therapy safe after a rotator cuff repair or should we delay PT to protect the healing tendons? Let’s dive into this and see what the research…
-

Knee Bracing Immediately After an ACL Reconstruction
I recently came across a Facebook post that discussed bracing immediately after an ACL reconstruction and I was intrigued. I read some of the comments and chimed in with my observations and opinions. In turn, a multi-platform discussion revealed many new details. I wanted to briefly share some of the research and the discussions that…
-
The Week in Research Review, etc 10-29-18
—
by
This week we started the week off with a couple shoulder posts, specifically the rotator cuff and SLAP tears. As usual, I can’t resist a good ACL paper so included that NM control program that should be in all knee patients’ programs. We ended the week with a recorded knee scope as the surgeon was…
-
The Week in Research Review, etc 7-29-18
—
by
Last week was the 1st of my research review that summarized my social media posts from the previous week. It seemed to be well received so I figured I’d continue it. My goal is to help summarize some of the research that I found interesting and package it nicely for my readers. Each photo contains…
-

2 Tips to Improve Your Post-op Rehabilitation Outcomes
I’ve treated hundreds, if not thousands of postoperative patients in my career. I’m always surprised to hear from others how they progress their patients. When I first got into physical therapy, I was all about protocols. I didn’t have much experience. I would literally follow it word for word and do my best to match…