Infraspinatus atrophy in a baseball pitcher with a UCL sprain
Infraspinatus atrophy due to a spinoglenoid notch cyst
This was an incidental finding of mine in a collegiate baseball pitcher. He presented with a UCL sprain during his senior year and was struggling.
He came in looking to salvage his senior year and attempt to pitch at some point. UCL surgery would’ve been warranted if he was anything but a senior.
UCL Evaluation
We evaluated his elbow and he presented with typical findings of painful valgus stress tests. I’ve discussed my UCL exam previously in a post that you can find here.
His shoulder PROM was slightly limited compared to what we normally see in our overhead throwers, which may have contributed to his elbow issues.
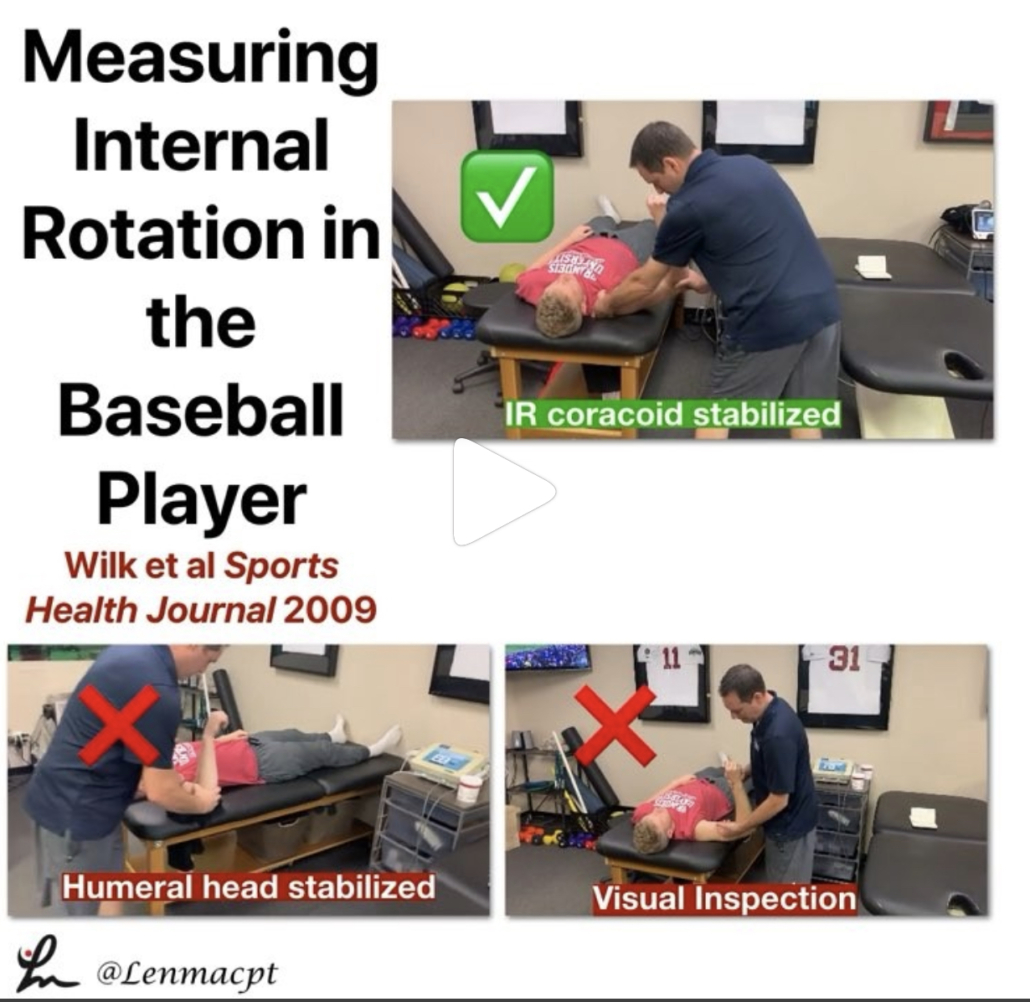
He only had 120 degrees of external rotation compared to 110 degrees on the right side. If you’re wondering how I measure external rotation, then this video below may be a good one to review.
We use these concepts for our research studies that we have published on weighted ball usage the past few years.
For those that will ask about GIRD, he had 60 degrees of IR on the L side and 50 degrees on the R side. I’m not a big GIRD guy like has been written by others. I still think GIRD is pretty normal and our research has shown that too.
Remember, we showed that differences in total rotational range of motion greater than 5 degrees was significant. This study was published in AJSM back in 2011.
Furthermore, we showed a connection between the loss of passive flexion and elbow injury.
This result was also shown by Camp et al in a separate study, as well.
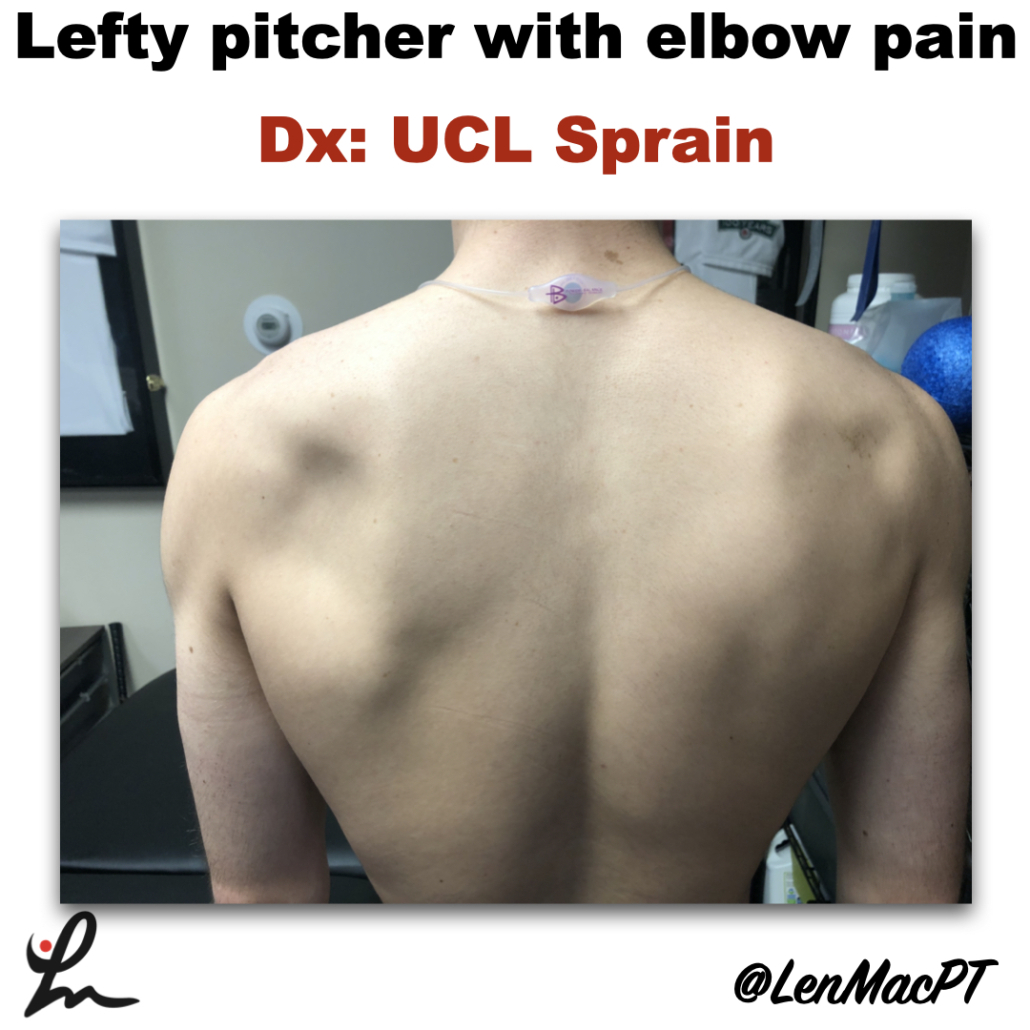
I had him remove his shirt and noticed a large defect in the infraspinatus area that showed obvious atrophy (see picture below).
The cyst was compressing the suprascapular nerve as it coursed along the spine of the scapula.
His external rotation strength was significantly weaker on his throwing side compared to his right side. This would make complete sense considering the amount of atrophy present.
Often times surgery is warranted to decompress the nerve. There’s often an underlying labral tear that has resulted in a cyst to form. The surgery would remove the cyst and repair the labrum to prevent future issues.
Quick Literature Review on Surgical Outcomes
Reports of improved outcomes are in the literature, here and here and here.
Obviously, this may have contributed to his elbow issues as the posterior cuff muscles are tremendous stabilizers of the arm, especially during the deceleration phase of throwing.
Treatment for infraspinatus muscle atrophy
Our goal was to calm the elbow down through active rest and focus on strengthening of his forearm and shoulder musculature.
We used neuromuscular electrical stimulation (NMES) to the infraspinatus. We felt as if the electrical stimulation would allow for a better muscle contraction than what he could do actively. This is a similar concept to using NMES to the quads after a knee surgery.
We have previously shown in AJSM that NMES to the infraspinatus was beneficial to patients after a rotator cuff repair. It helped improve their muscle contraction by 22% in the group with the NMES applied during testing.
Outcomes and final thoughts
Believe it or not, we were able to salvage his senior year despite all of the issues that presented.
He made numerous pitching outings and was pretty successful for his team.
The lesson here: Don’t take anything for granted, observe and test.
Make sure you look distal and proximal. It could’ve been very easy to just treat the elbow with some exercises and massage. Don’t get me wrong, we did a bunch of strengthening exercises to his forearm.
His secondary finding was most likely a leading cause for his elbow dysfunction.
This isn’t the 1st time that I’ve run across an issue like this. I’ve found numerous scapula dysfunctions like this involving the infraspinatus. But also a winging issue due to a long thoracic nerve palsy.
You must look at the whole picture… shirts off for a guy and a sports bra for a female to make sure we’re not missing anything obvious!