The Week in Research Review, etc 12-10-18
This week we’re still playing with formats and learning these Instagram changes. With that, in the week in research review 12-10-18, we discussed many topics that I wanted to share!
Surgery vs Physical Therapy for Carpal Tunnel Syndrome
Cost-Effectiveness Evaluation of Manual Physical Therapy Versus Surgery for Carpal Tunnel Syndrome: Evidence From a Randomized Clinical Trial Fernández-de-las-Peñas et al JOSPT 2018.
This Level 1b study looked to evaluate cost-effectiveness differences of manual physical therapy versus surgery in women with carpal tunnel syndrome (CTS).
Performed in Spain, 120 women with a clinical and electromyographic diagnosis of CTS were randomized through concealed allocation to either manual physical therapy or surgery.
They concluded that manual PT including desensitization maneuvers of the central nervous system has found to be equally effective but less costly, i.e., more cost-effective than surgery for women with CTS.
From a cost-benefit perspective, the proposed manual PT intervention of CTS can be considered.
Interesting results but 2 obvious limitations to this study:
1️⃣No control group. What if the symptoms could spontaneously improve over time
2️⃣ They only looked at 1-year improvement and not short-term improvements. I would’ve liked to have seen 3 months and 6 months results as well to see the acute effects.
Not sure what to make of this study but it does seem as if a population of Spanish women may respond to Rx of CTS without surgical intervention.
This could be a huge cost/time saver for society!
Return to Sport Criteria and Reinjury Rates
The Association Between Passing Return-to-Sport Criteria and Second ACL Injury Risk: A Systematic Review With Meta-Analysis Losciale et al JOSPT 2018.
Not going to lie, this study caught my attention because the results match my confirmation bias.⠀
I’ve been saying for years that hop tests, even combined with other tests, just don’t cut it.⠀
I wrote a blog post about this too for @mikereinold. This study, although with its limitations, did show that passing RTS criteria did not show a statistically significant association with risk of a second ACL injury.
This review also determined that 12% of those who failed RTS testing suffered a graft injury, compared to 5.9% of patients who passed.
It seems as if quadriceps strength measured via isokinetic testing or isometric testing may be an important factor to consider for RTS decision making.
Also, hamstring-quadriceps strength ratio symmetry should also be considered.
So with this review demonstrating that current objective criteria-based RTS decisions did not show an association with the risk of a second ACLI, how does this affect your practice?
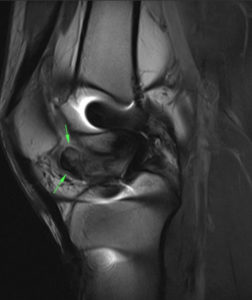
Physical Therapy vs Knee Scope for Meniscus Tears
💥PT vs Scope for Meniscus Tear 💥
.
Effect of Early Surgery vs Physical Therapy on Knee Function Among Patients With Non-obstructive Meniscal Tears: The ESCAPE Randomized Clinical Trial. van de Graaf VA et al JAMA Oct. 2018
Among patients with non-obstructive meniscal tears, PT was equal to arthroscopy for improving patient-reported knee function over a 24-month follow-up period.
They went on to say that “Based on these results, PT may be considered an alternative to surgery for patients with non-obstructive meniscal tears.”
So basically, if there’s no bucket handle tear present that may be blocking joint range of motion, then it is highly encouraged that the patient #GetPT1st and not do surgery.
Without going out on a limb, I’d say this is a much
I do note a couple limitations: the surgical group did not get PT after surgery if they did ‘as expected’ but they could get PT to help improve their symptoms.
The PT group did pretty basic exercises although leg press, lunges, and balance type exercises were included.
Have you read this paper? It was a multi-center, randomized controlled trial performed in 9 hospitals in the Netherlands.
So, are we encouraged or surprised? Let me know by commenting below…thanks!
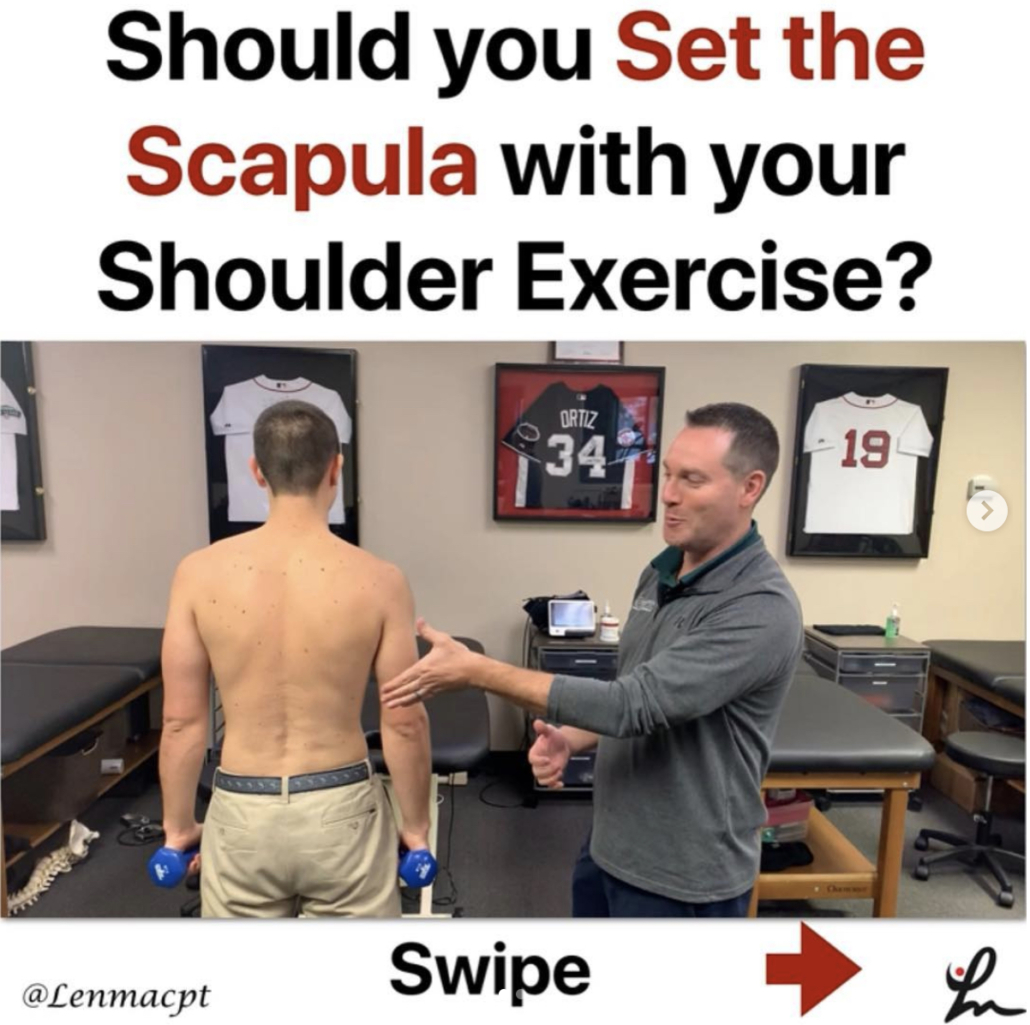
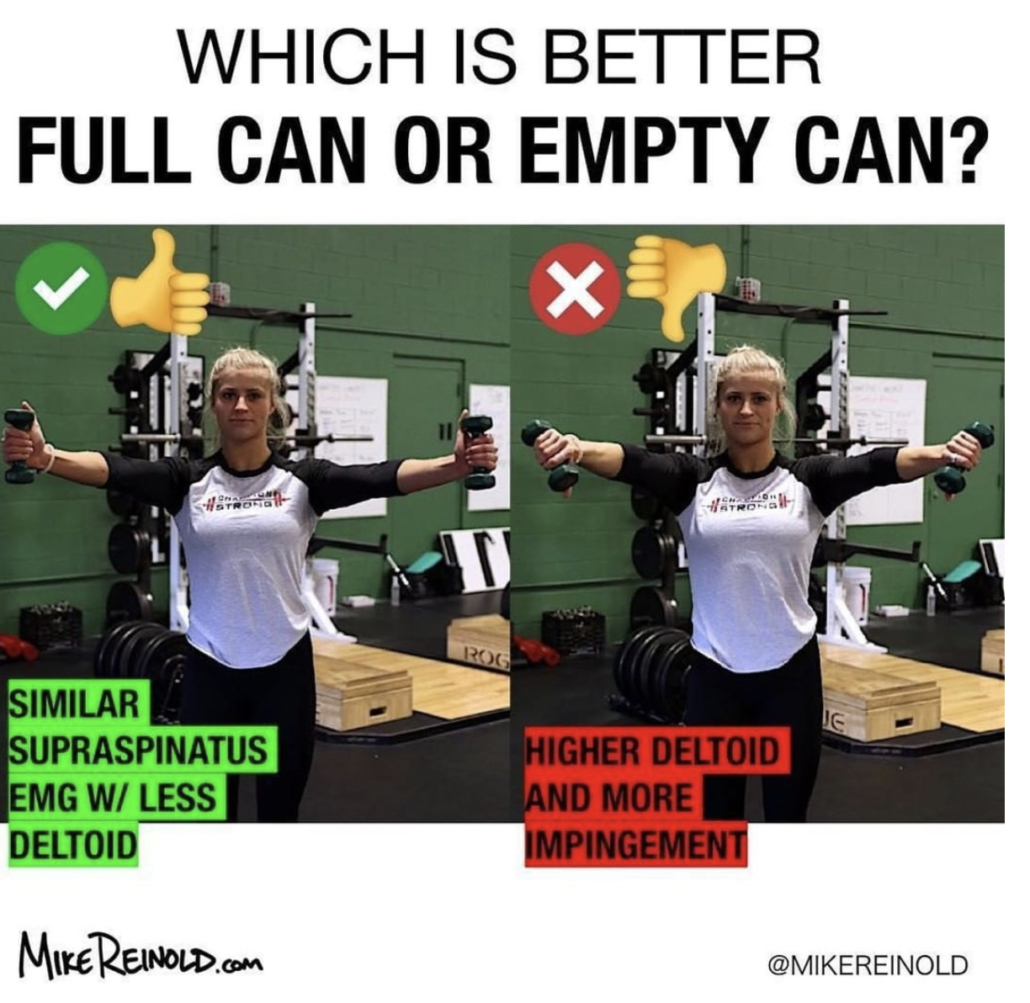
Shoulder Health Accessory Exercises
by @kieferlammi
Want strong and healthy shoulders!?
Shoulder strength is about more than pushing big lifts like strict pressing, push pressing, etc.
If you want a robust, healthy, well moving shoulder you should be including lower level drills that more specifically address scapular and RTC strength and control. –
I will always be a fan of traditional exercises like side like ERs, Prone Ys, Ts, etc.
Lately, I’ve thrown in more band work because it’s easy for me to do for higher volumes on a frequent basis and I enjoy the constant tension that the band provides.
Give these two exercises a try:
✅ Band Front Raise Pull-Apart
✅ Band Overhead Y Raise
I find that these two do a great job of targeting my mid back and posterior shoulder without much compensation through a big range of motion.
Give them a try either in a warm-up for 1-3 sets of 10-15 reps or at the end of a training session for 2-4 sets of 10-25 reps depending on the difficulty of your band and your capacity.
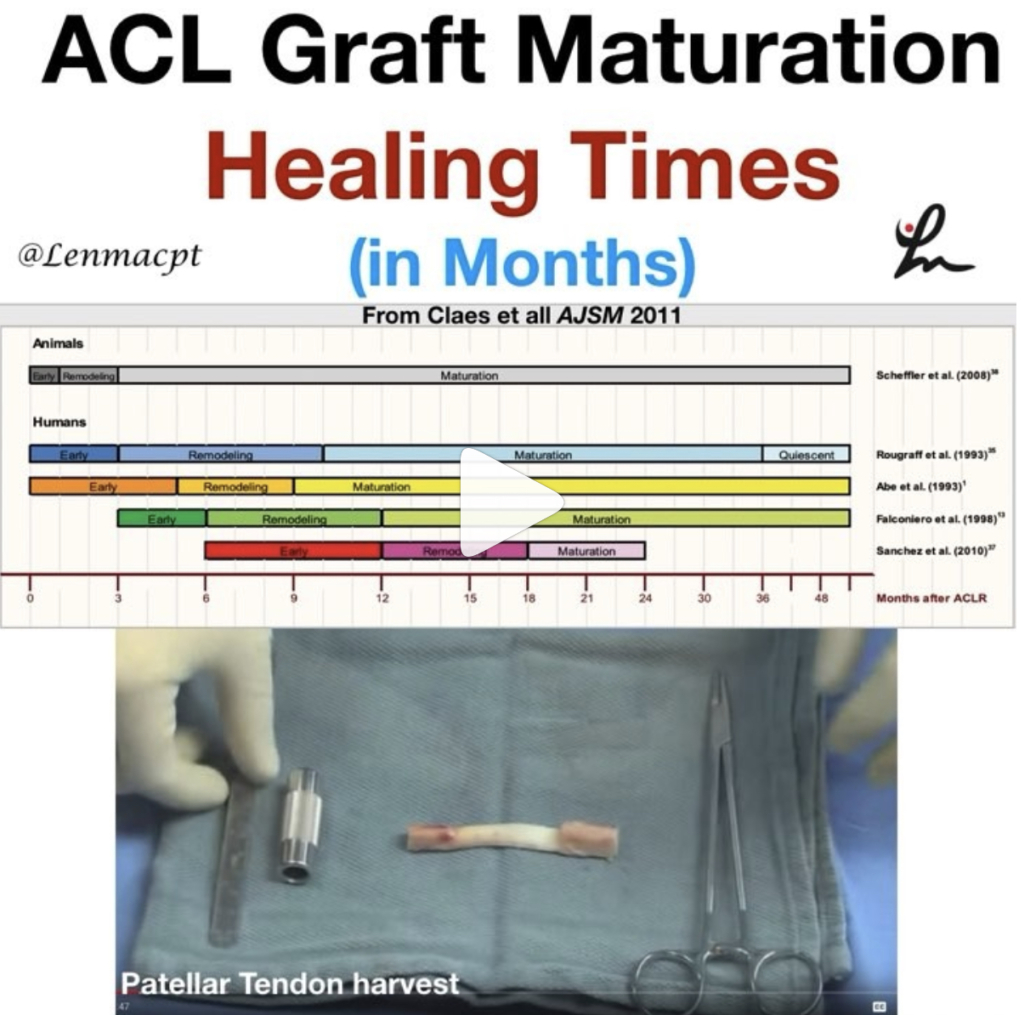
Should we Brace after an ACL Surgery?
You can also get to the blog post by clicking this link
Let me know what you think about this new blog post or any of my social media posts…thanks!