Why you need “Feel” as a Physical Therapist
I haven’t written a post in a while but wanted get back into the swing of things. In this post, I wanted to talk about having ‘Feel’ as a PT.
When I say feel, I’m talking about being able to read people and adjust the situation based on their response to things. So, what does that mean? Not really sure… but wanted to give a few examples that I have heard recently that I think happen pretty commonly in our profession.
Exercise Progression (or lack of)
This one happens a bunch in our profession and I was guilty of this early on in my career. It’s much easier to have someone come in 2-3 times per week and give them the same exercises, right? But to do this for multiple weeks, if not months, is a travesty!
Listen, I don’t think we need to progress someone’s program every session. Adding a new exercise each visit can be a bit much. know we want to make people feel as if they are moving forward in their rehab but there are other ways we can progress people besides giving them 17 different exercises that keeps them in PT for 2+ hours.
Again, I was guilty!
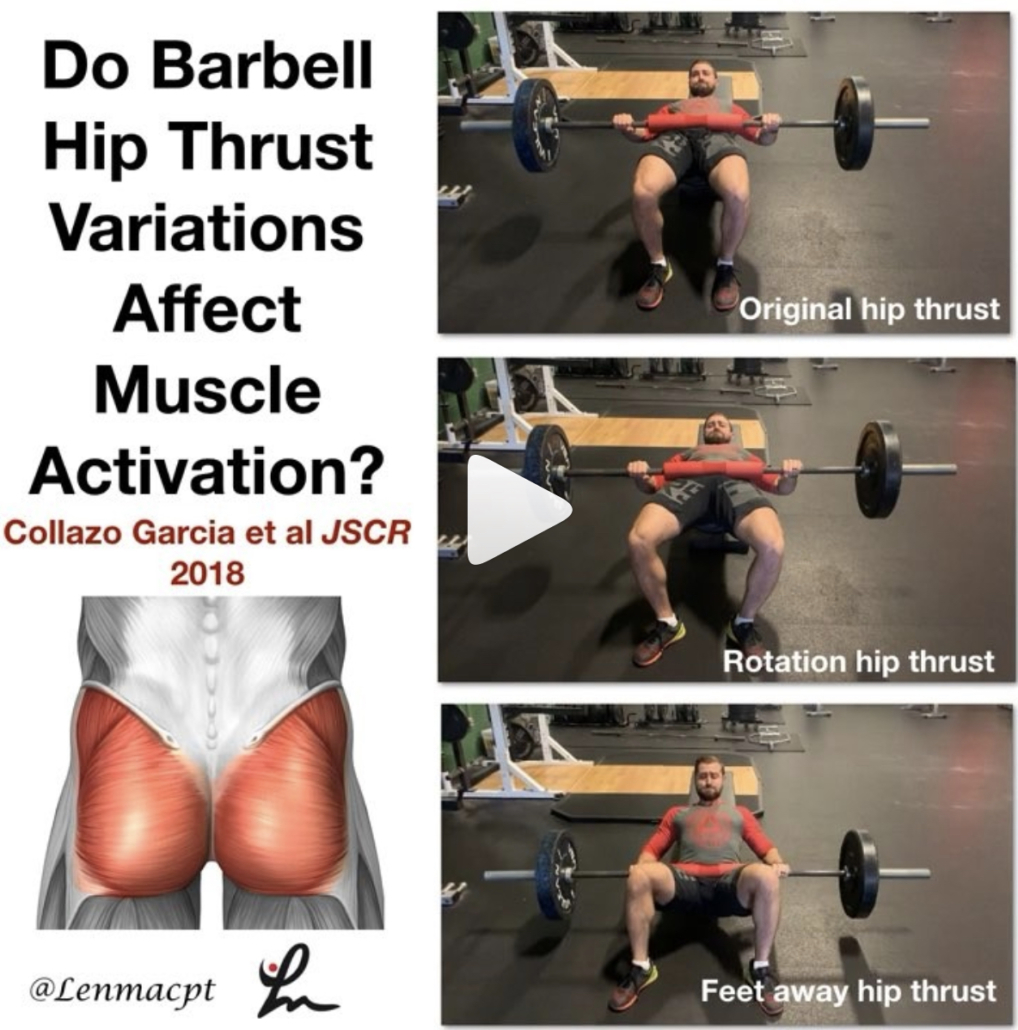
There are so many variables that we can manipulate for each session, it’s silly! Think about each move that someone does and break it down.
Exercise Variables to Manipulate
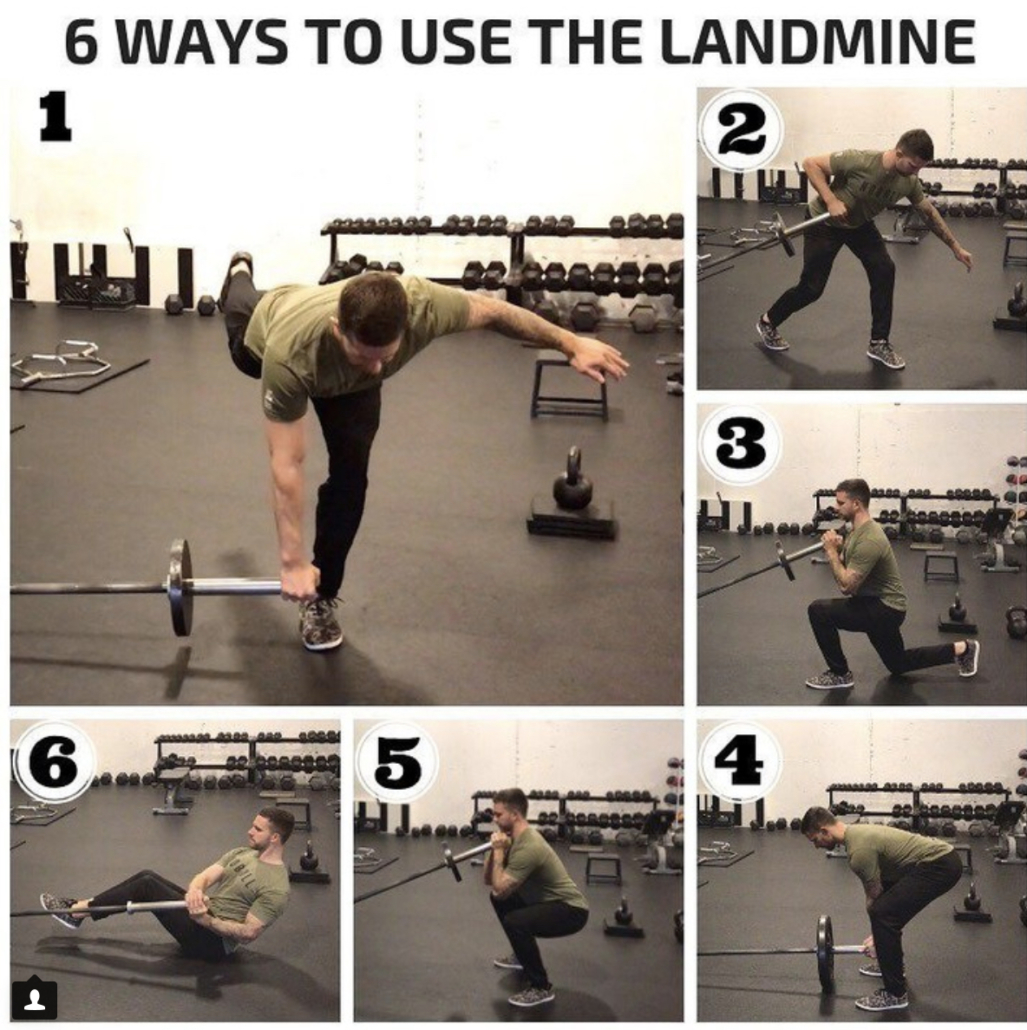
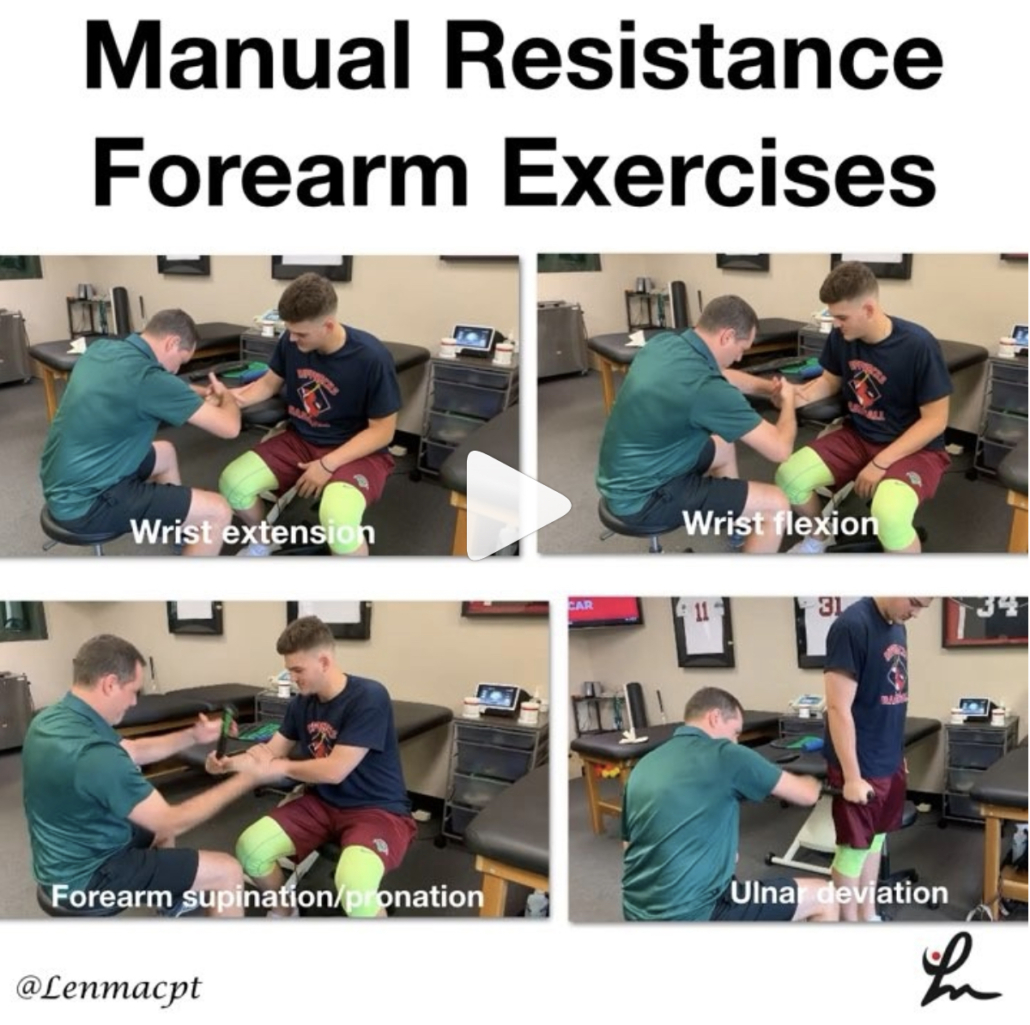
We can play with:
- Tempo
- Single leg versus double leg
- Reps/sets scheme
- Upper body or lower body
- Time under tension
- External resistance (bands, chains)
- Rest periods between exercises
- Perceived RPE (stole that one from Kiefer!)
- Volume
So as you can see, even if you don’t have heavy weights as we do here at Champion PT and Performance, then you can still get creative with progressions.

Personally, my clients have the same program for 4 weeks and then we write them a new program. That means that they can focus on the aforementioned variables as needed even though they are doing the same exercises for 4 weeks.
The client likes it because they get really good at that movement plus they can see their progression in their weights, which is a huge mental gain!
Besides the obvious weight progressions, there’s a ton that can be manipulated but I don’t see or hear it enough from the patients that come through here. I rarely hear a client tell me that their previous PT experiences involved any type of variable manipulation but maybe that’s why they find us in the 1st place. Who knows…
My advice, let the patient feel as if they are moving forward in their exercise prescription because they are a smarter consumer than you would think. As PT’s we must do better with this stuff and the above bullet points are a good starting point for you.
Running on Empty
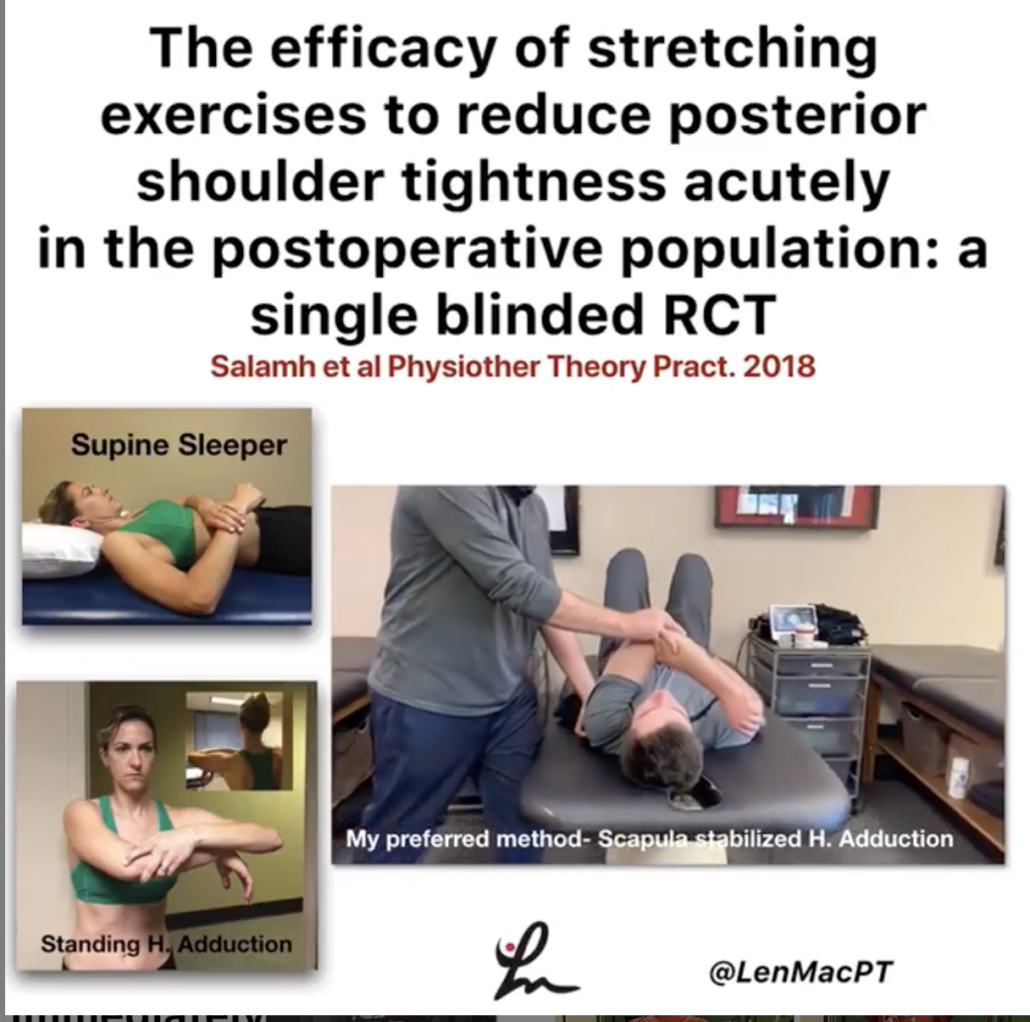
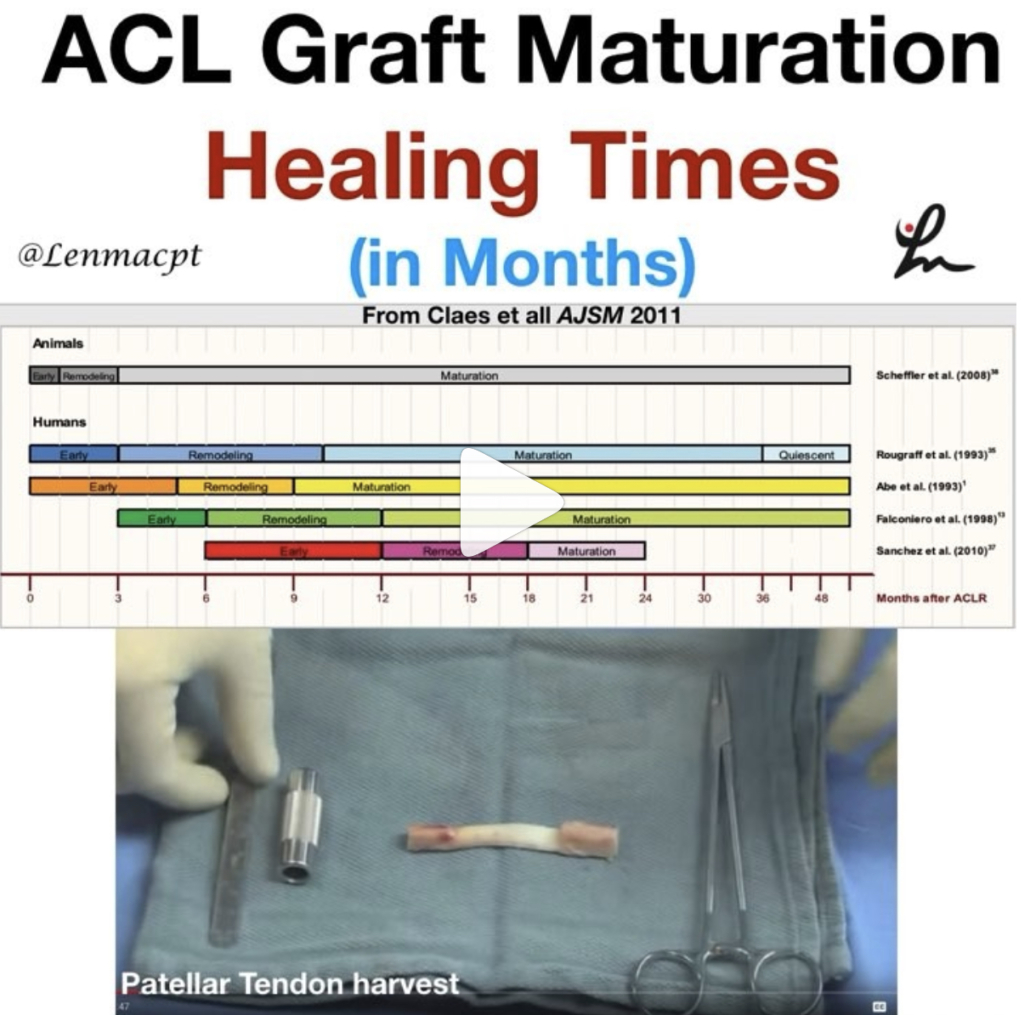
On another note, I recently started treating someone for a knee injury she sustained while skiing. Fortunately, she didn’t require surgery but the fracture needed time to heal. I don’t want to reveal too many details of the case for privacy reasons but just know she could’ve easily done more damage to her knee from the mechanism of injury.
She was given a brace and a prescription for PT to begin immediately for ROM and strengthening. She was limited in weight bearing for a period of time (I don’t remember the exact amount) so she had those effects that she had to deal with too.
At the beginning of the 6th week after the injury, her doc said she was fine to begin running even though no new x-rays were done on her knee. Guess they were just going off of time and that she was a healthy female without any co-morbidities.
Back at PT, she was told to start a running program that she thought was a bit early but she was excited to progress to more aggressive exercises.
According to her, she had been doing straight leg raises, clams, bridging and other low-level exercises for the whole duration of the rehab…see above rant!
Upon beginning her running program, she felt immediate pain and had to stop. She said she felt bad because the PT was surprised that the pain was still present but she wanted to work through it a bit. Despite trying to push through it, she still felt pain and had to stop again. She felt a big sense of failure because the pain persisted and she just couldn’t get over this hump.
Think Mode
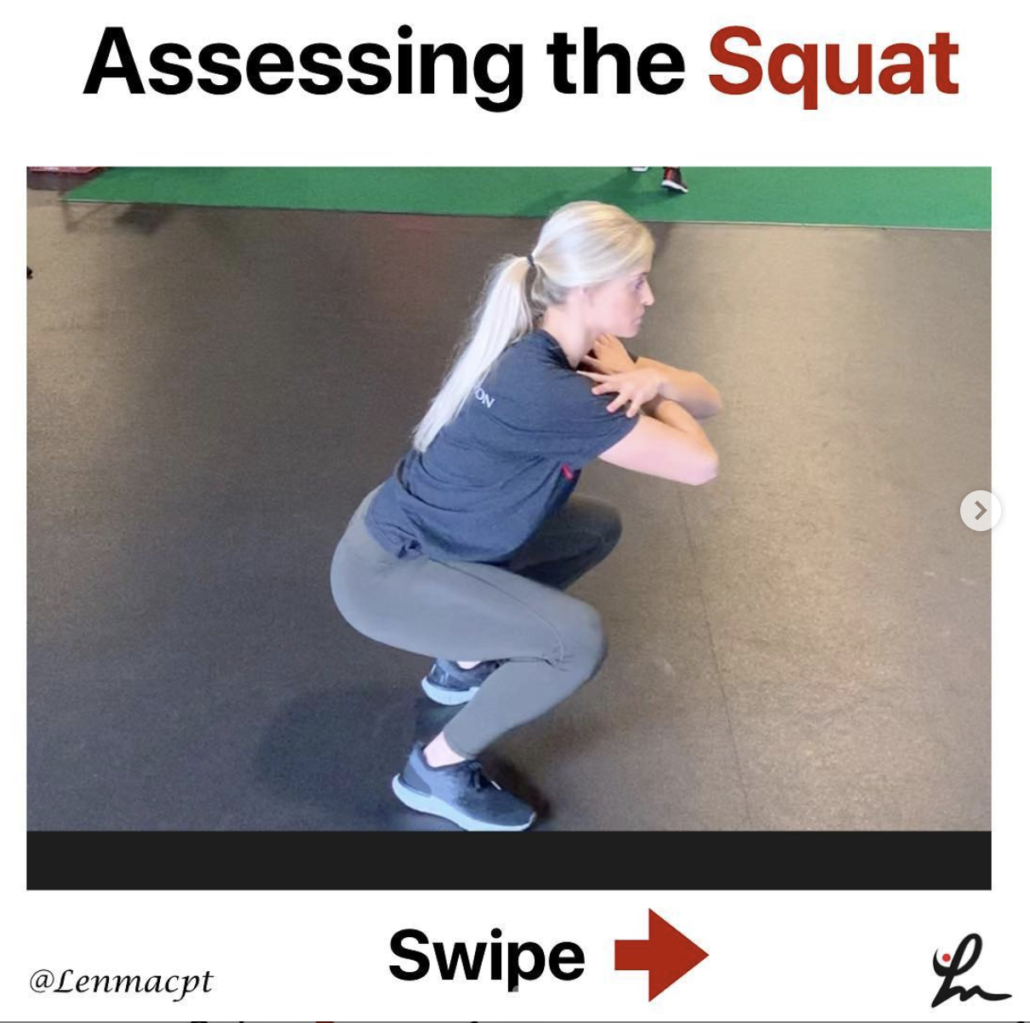
Let’s think about this scenario for a second. Six weeks after a joint fracture, little strength training after a decent period of immobilization and the patient was expected to run?
As it turns out, the patient was frustrated enough with the scenario that she sought a second opinion and found us. I’ll never put down another PT’s plan of care but it was obvious that the plan was rushed and the patient’s opinions and communications were not fully observed.
She was frustrated and felt defeated but why? Why would someone be expected to run 6 weeks after a fracture without loading the joint and going through a progressive program?
I’m not sure but I wanted to use this case as a teaching moment for other clinicians, especially the younger crowd that may struggle with rehab progressions.
Listen Up!
Listen to the client and have a good understanding of basic soft tissue healing. I told the client that she needed a good 6-8 weeks of strength training before even talking about running. She was relieved that I wanted to take it slow and we now have a very happy client who has completely bought into my system.
Again, listen to your clients. They’ll tell you what’s wrong with themselves if you listen closely!
My Dad’s Knee Replacement
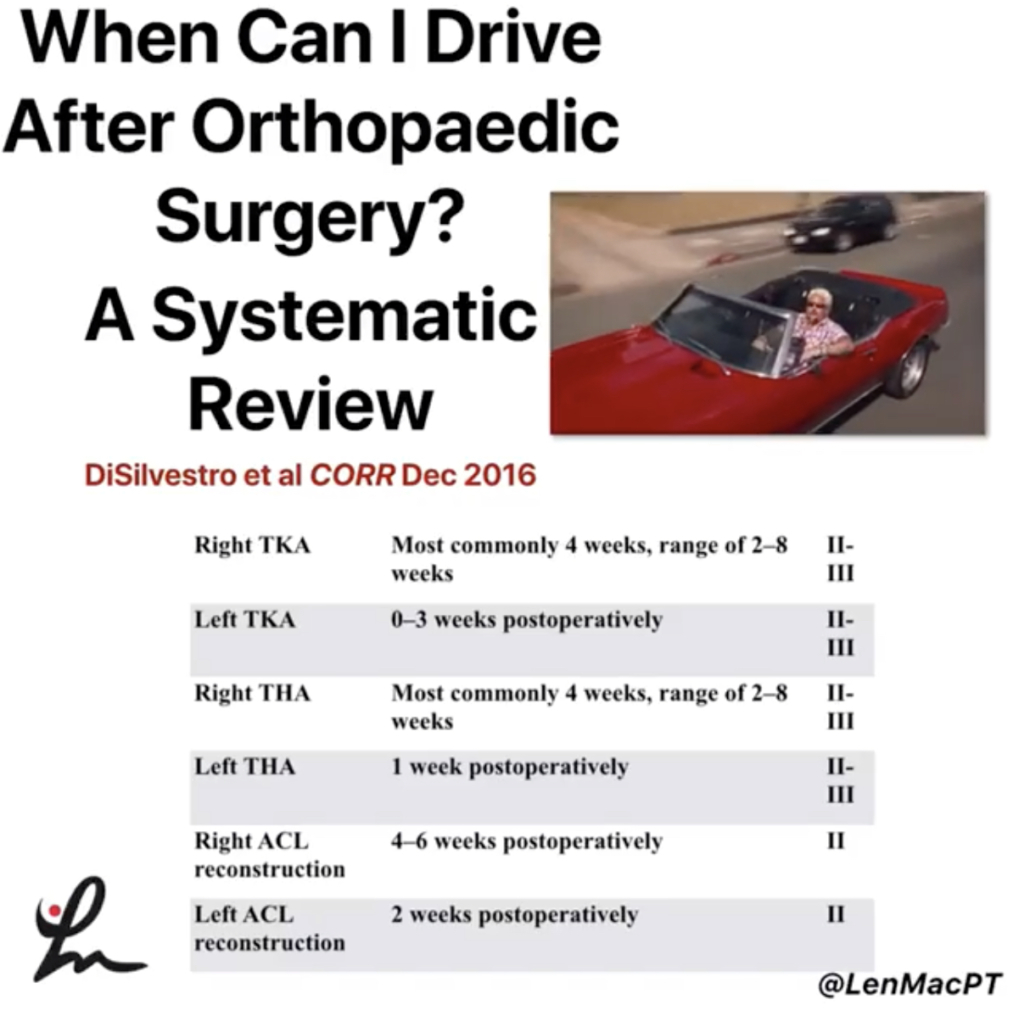
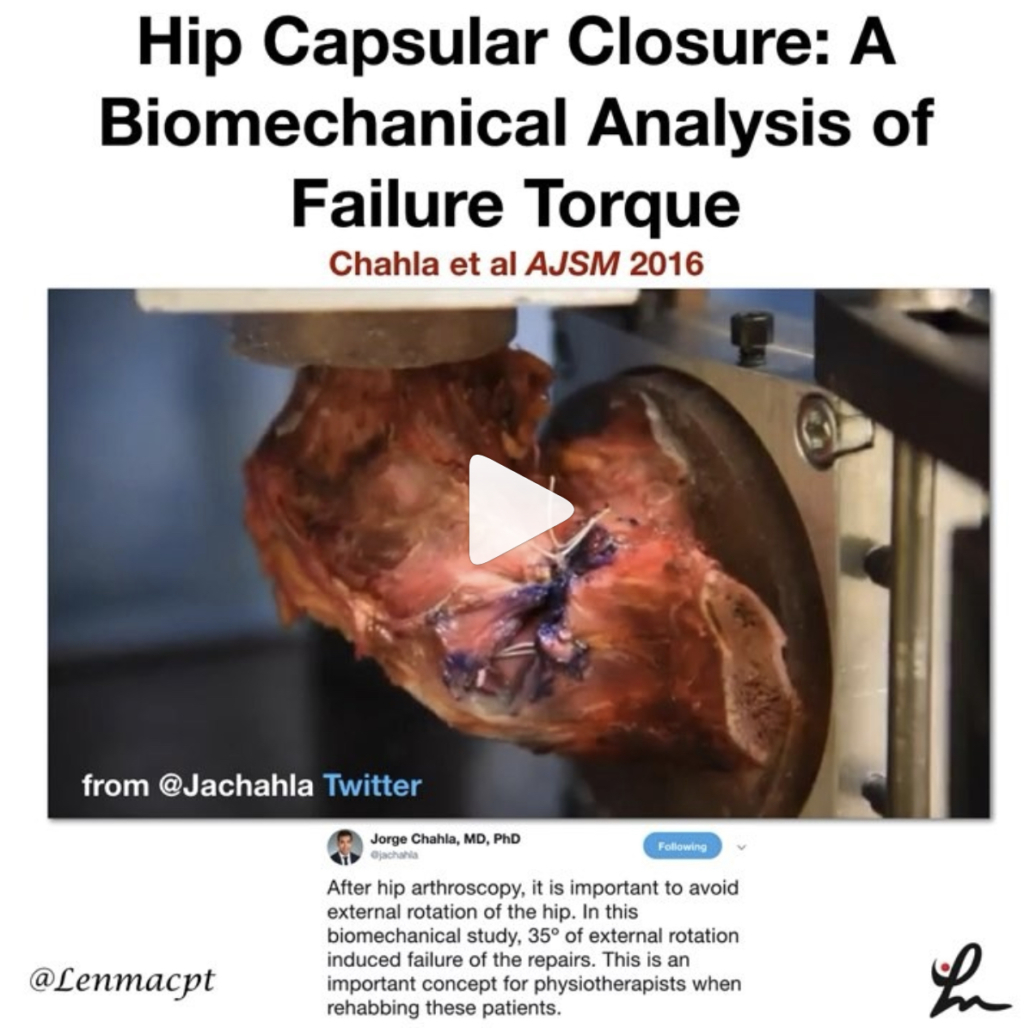
Switching gears, my Dad has his knee replaced a few weeks ago. Despite having treated a gazillion knee patients in my career, my Dad has yet to step foot in our facility. I’ve given him advice from a distance and have tried to keep an eye on things as they came up.
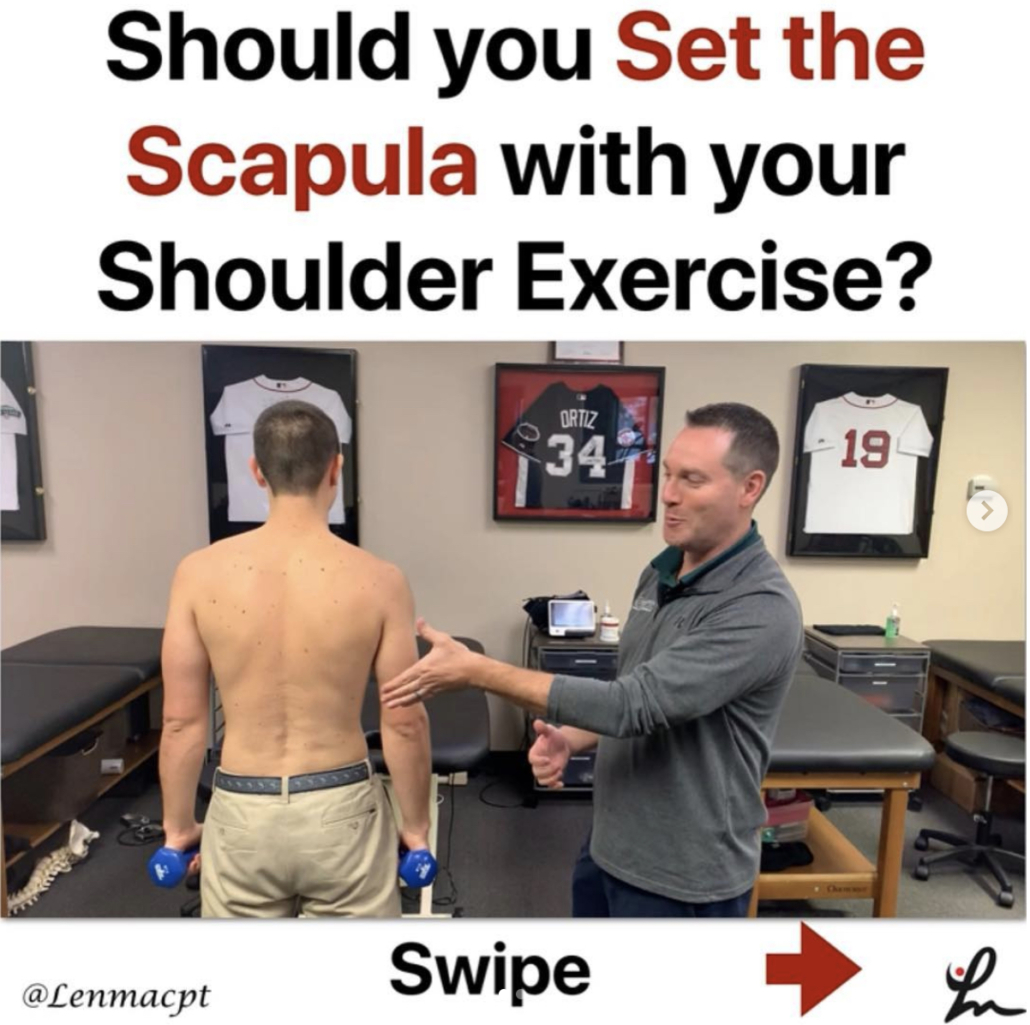
I’m not a home health PT and respect their jobs. I was surprised that no one ever tried to bend his knee during the home visits he had for nearly 6 weeks. Fortunately, he had about 80-90 degrees of flexion but the home health PT kept telling him he didn’t need more than 90 degrees of motion.
You try to get up from a chair with only 90 degrees of knee flexion! I’ll bet it’s much more difficult than 110+ degrees of motion. For the record, I shoot for 120 degrees of knee flexion ROM for all.
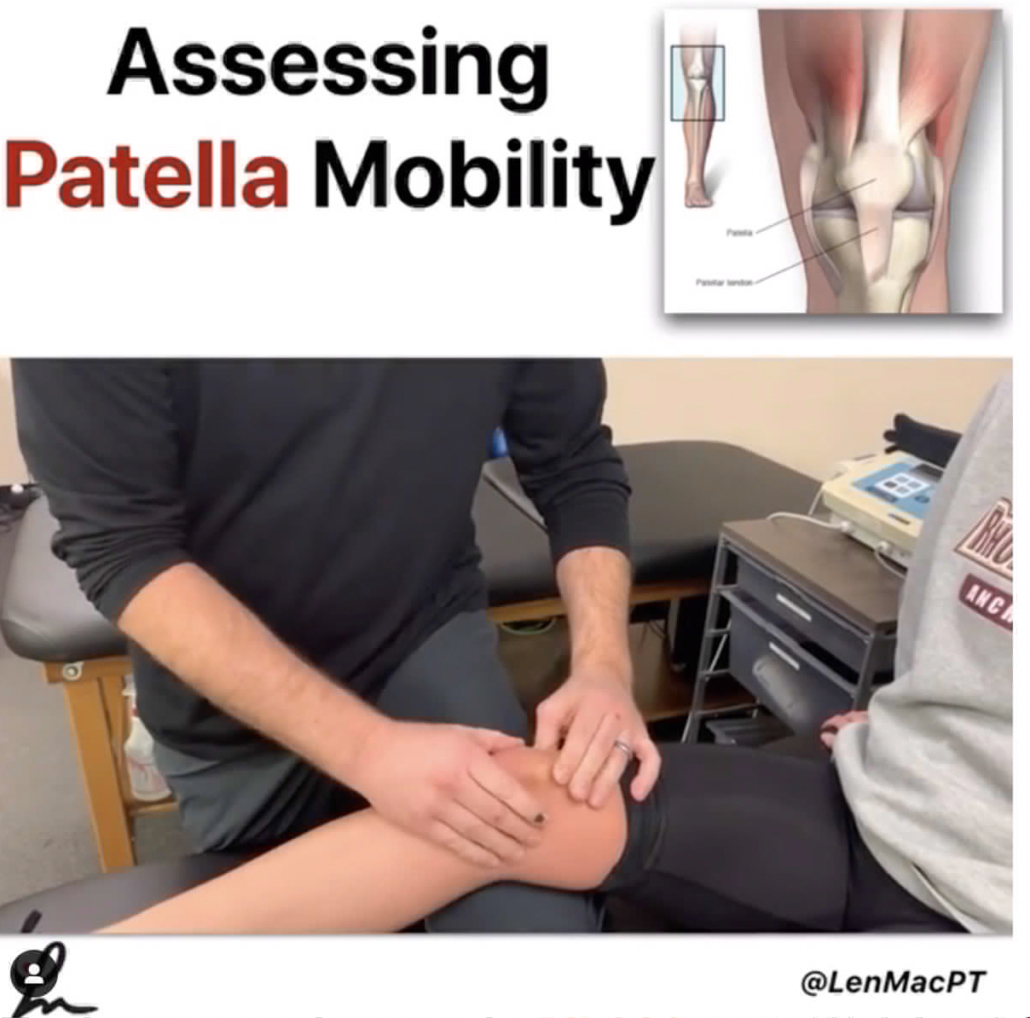
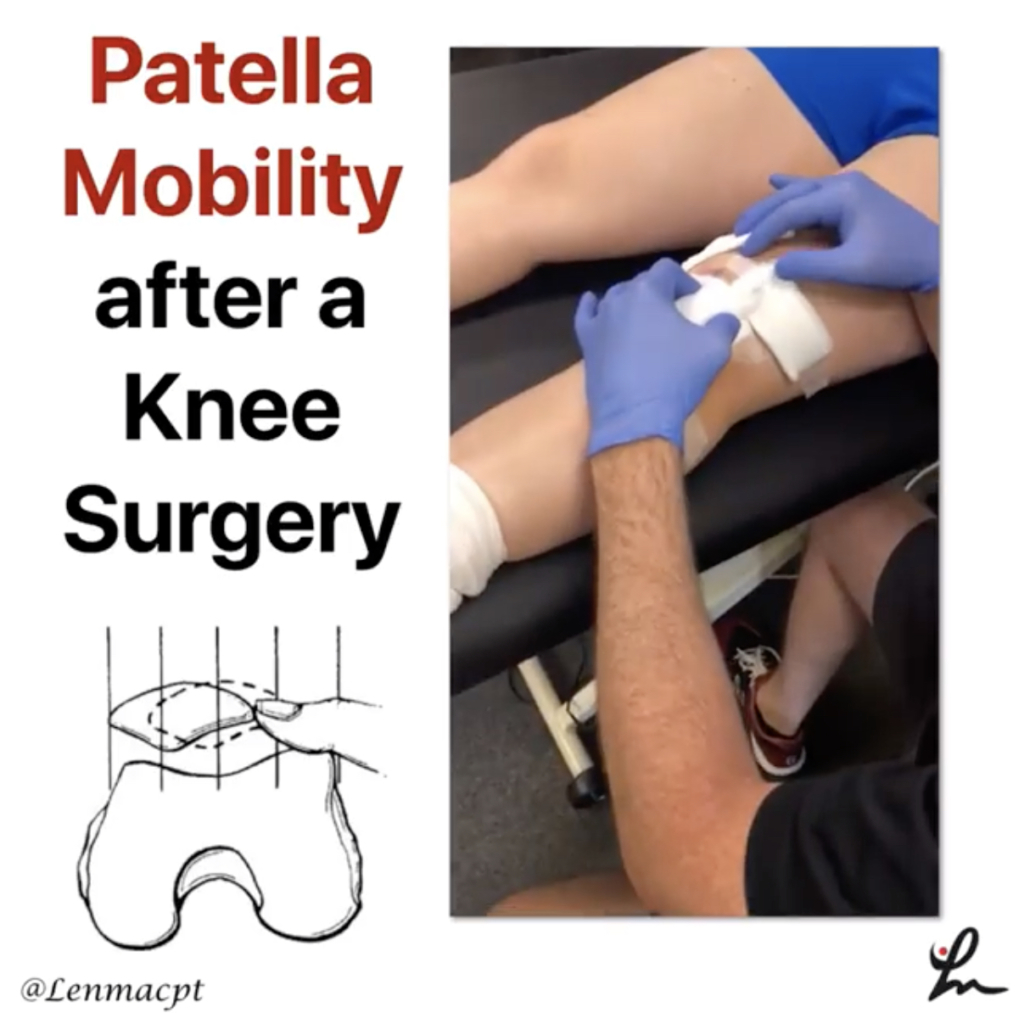
After home health, my Dad started outpatient PT and he sounded confident and happy. Yet again, no one felt the need to bend his knee (he did get some patella mob’s) and just showed him basic exercises like straight leg raises and squats.
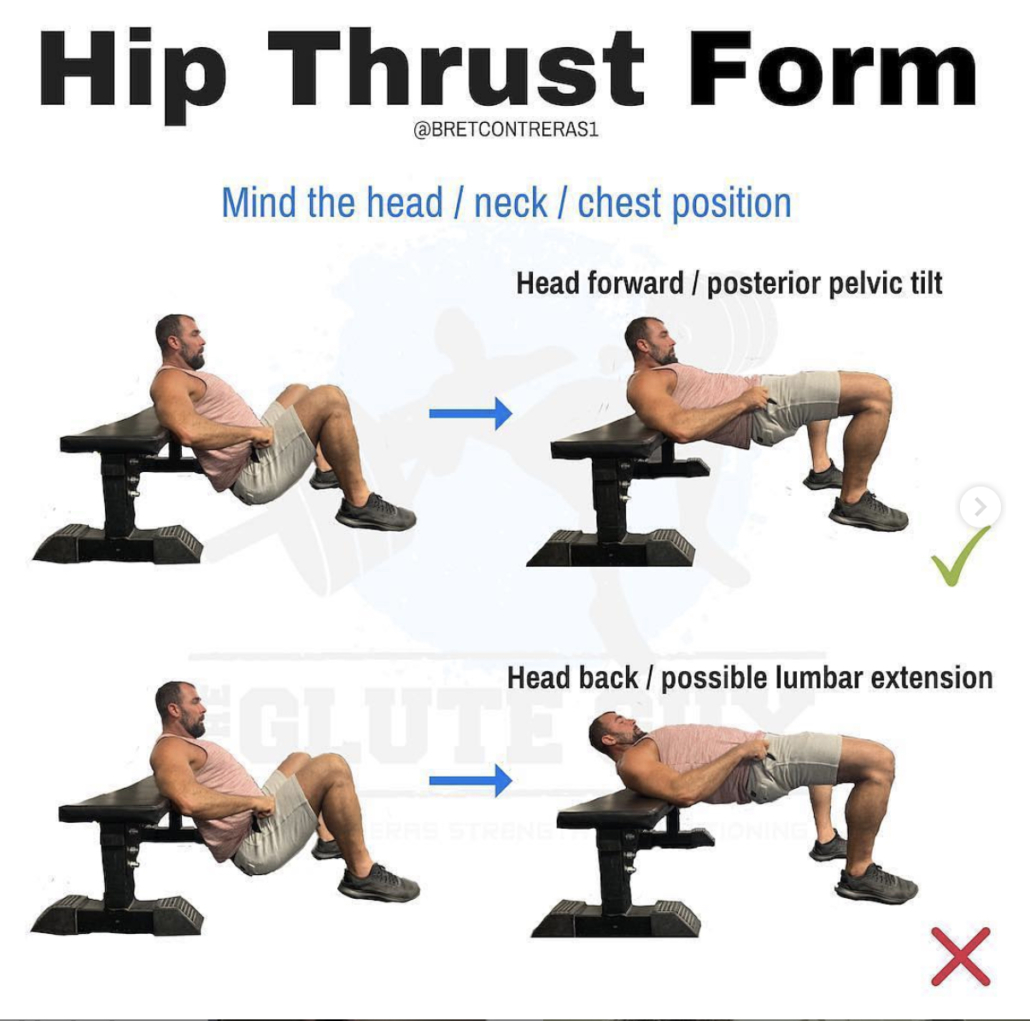
Obviously an important component to PT but I still think getting more ROM is critical. I’ve talked about how I like to bend the knee after surgery at my YouTube channel that you can access here. As you can see, I prefer the seated position at the edge of the table for its comfort and isolation of the knee joint without hip compensation.
However, no one is bending his knee and he was feeling stiff. He did get a new PT for one of his sessions and they did bend his knee but only 2 times…and each time they cranked on it to the point he had to tell them to stop because of the pain.
Not how I would’ve initiated ROM!

He’s now 3 days after the PT session and frustrated. He told me he can’t do anything around the house anymore and has considered taking pain medication to help get over the hump. This is the ‘feel’ that I’m talking about.
Why on Earth would any PT think this technique would be beneficial? I’ve heard this way too often in the past and am frustrated by it.
If that were you 🤔
My advice…as always, put yourself in their position and consider the risk/reward. Is this the best we can do and will the patient absolutely benefit from this?
In my Dad’s situation(s) I say he has received mediocre care so far. Fortunately, I have guided his home program and have tried to keep him positive and realistic.
He’s frustrated and vows to never consider his other knee even if he can’t walk. I hope he changes his mind once he gets stronger and more functional.
My lesson in this post- listen to the client and do what’s in their best interest. Have some FEEL and progress people more appropriately.
We can do better!