The Week in Research Review, etc 10-29-18
This week we started the week off with a couple shoulder posts, specifically the rotator cuff and SLAP tears. As usual, I can’t resist a good ACL paper so included that NM control program that should be in all knee patients’ programs. We ended the week with a recorded knee scope as the surgeon was mobilizing the patella. It was a very informative and fun way to see the patella. We closed the week off with an old school video of myself performing a proprioception drill for the shoulder. I recommend you read these posts and like them on Instagram. Take a look at The Week in Research Review, etc 10-29-18
- Topics on the Rotator Cuff including post-op
- Classifying SLAP tears
- Essential Components of a neuromuscular control program
- Live Patellar scope during mobilization
- Shoulder Proprioception Drill
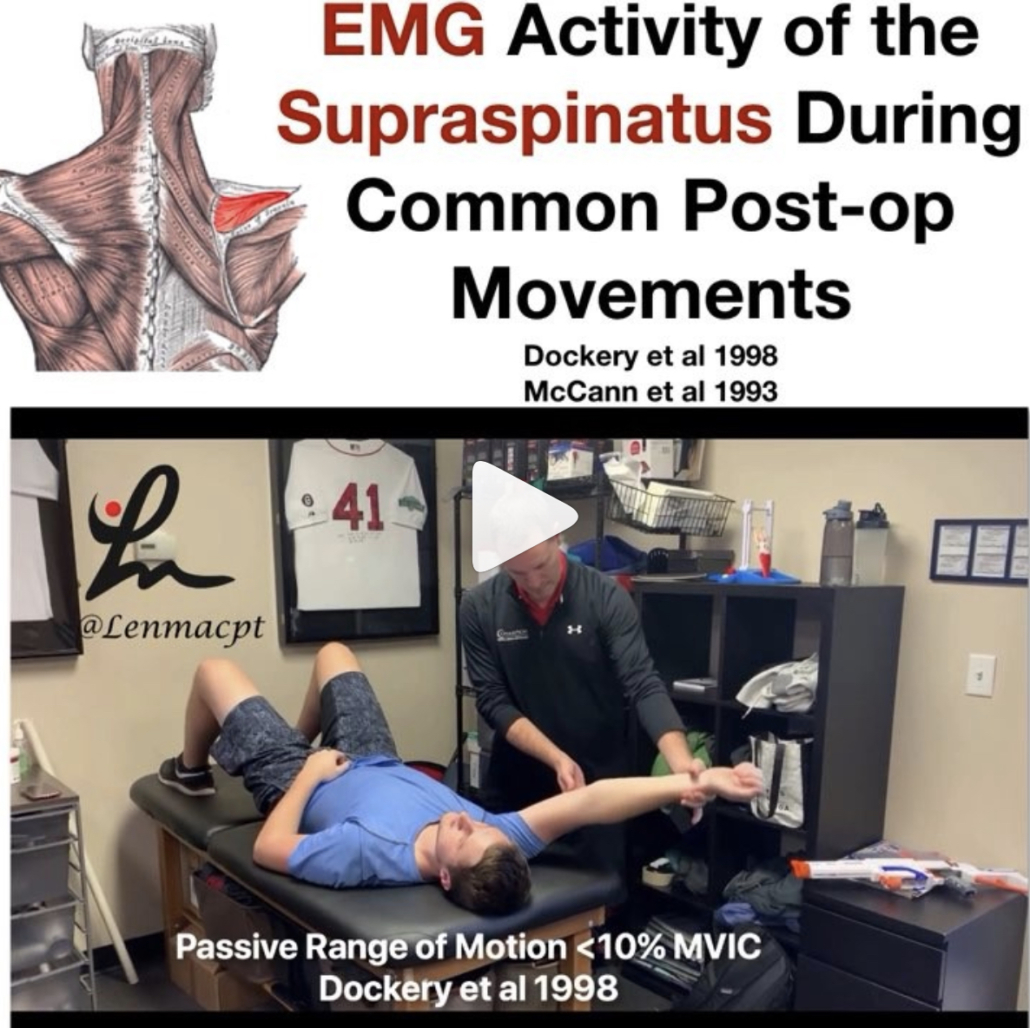
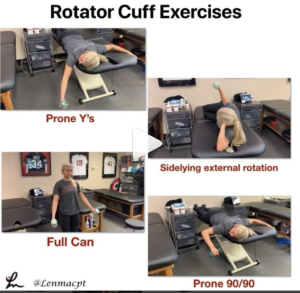
Topics on the Rotator Cuff including post-op
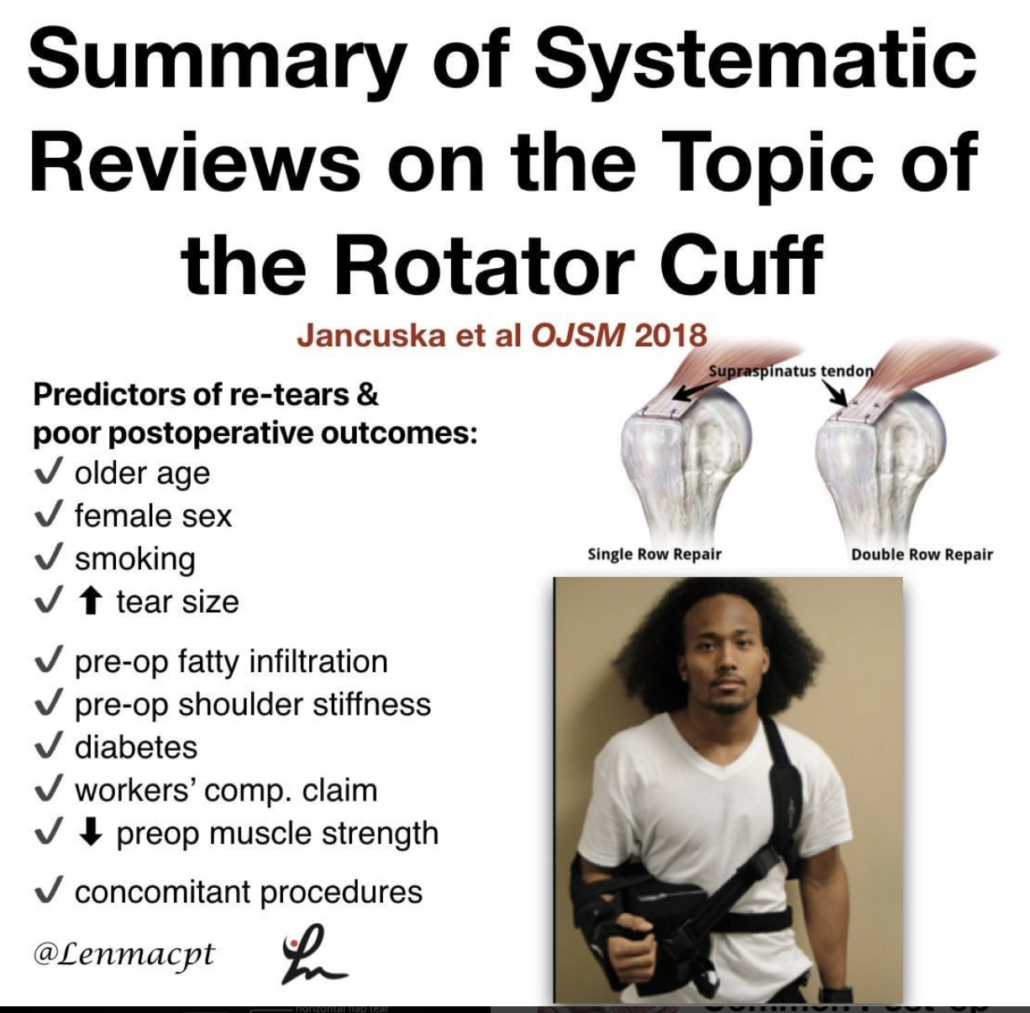
A Systematic Summary of Systematic Reviews on the Topic of the Rotator Cuff- Jancuska et al OJSM 2018
Nice summary of systematic reviews for you guys if you treat patients after a rotator cuff surgery. I’ve been doing a pretty good literature on the topic and wanted to share some of the articles that I have found helpful.
Their conclusions:
❇️There is substantial evidence indicating that the most accurate physical examinations for diagnosing RC tears are a positive painful arc and positive ER lag test
❇️Considerable evidence showing that rehabilitation is better than no rehabilitation for non-op management of RC tears, although RC repair was shown to be superior to rehabilitation alone.⠀
❇️No evidence to support the use of injections for nonoperative management of RC tears.
❇️Double Row repair results in better outcomes and fewer re-tears than Single Row repairs, especially for tears >3 cm.
❇️Predictors of re-tears and poor postoperative outcomes:⠀
✔️older age⠀
✔️female sex⠀
✔️smoking⠀
✔️increased tear size⠀
✔️preoperative fatty infiltration⠀
✔️preoperative shoulder stiffness⠀
✔️diabetes⠀
✔️workers’ compensation claim⠀
✔️decreased preoperative muscle strength⠀
✔️concomitant procedures.
Overall, a good review of the literature on rotator cuffs and anything associated.⠀
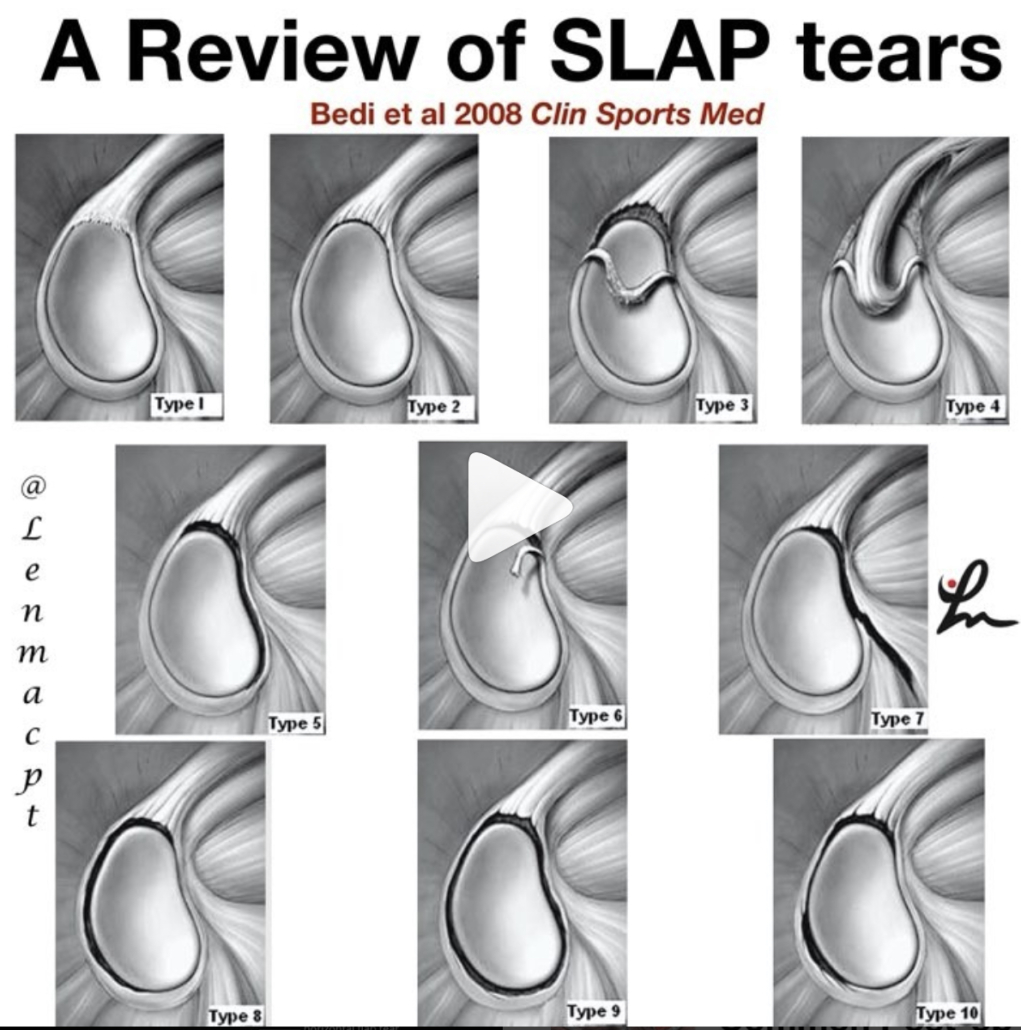
Classification of SLAP Tears
If you treat patients with shoulder pain, then you may run into different labral tears of the shoulder.
This post hopes to summarize the 10 different types of #SLAP tears that are currently known.
Type 1️⃣: Fraying but intact biceps
Type 2️⃣: Superior Labrum and biceps detached from the glenoid rim
Type 3️⃣: Bucket handle tear of the superior labrum but biceps anchor attached
Type 4️⃣: Bucket handle tear of the superior labrum that extends up into the biceps tendon
Type 5️⃣: BankartTear and also a detached biceps anchor
Type 6️⃣: an unstable flap of the superior labrum with a detached biceps anchor
Type 7️⃣: Anterior superior labral tear that extends to the middle Glenohumeral ligament; Biceps anchor detached
Type 8️⃣: Superior and posterior labral tear along with detached biceps anchor
Type 9️⃣: 360° labral tear
Type 🔟: Superior labral tear along with reverse Bankart tear and a detached biceps anchor.
That’s a lot and some are pretty rare but it helps to be able to communicate effectively with the medical team or to read an operative report.⠀
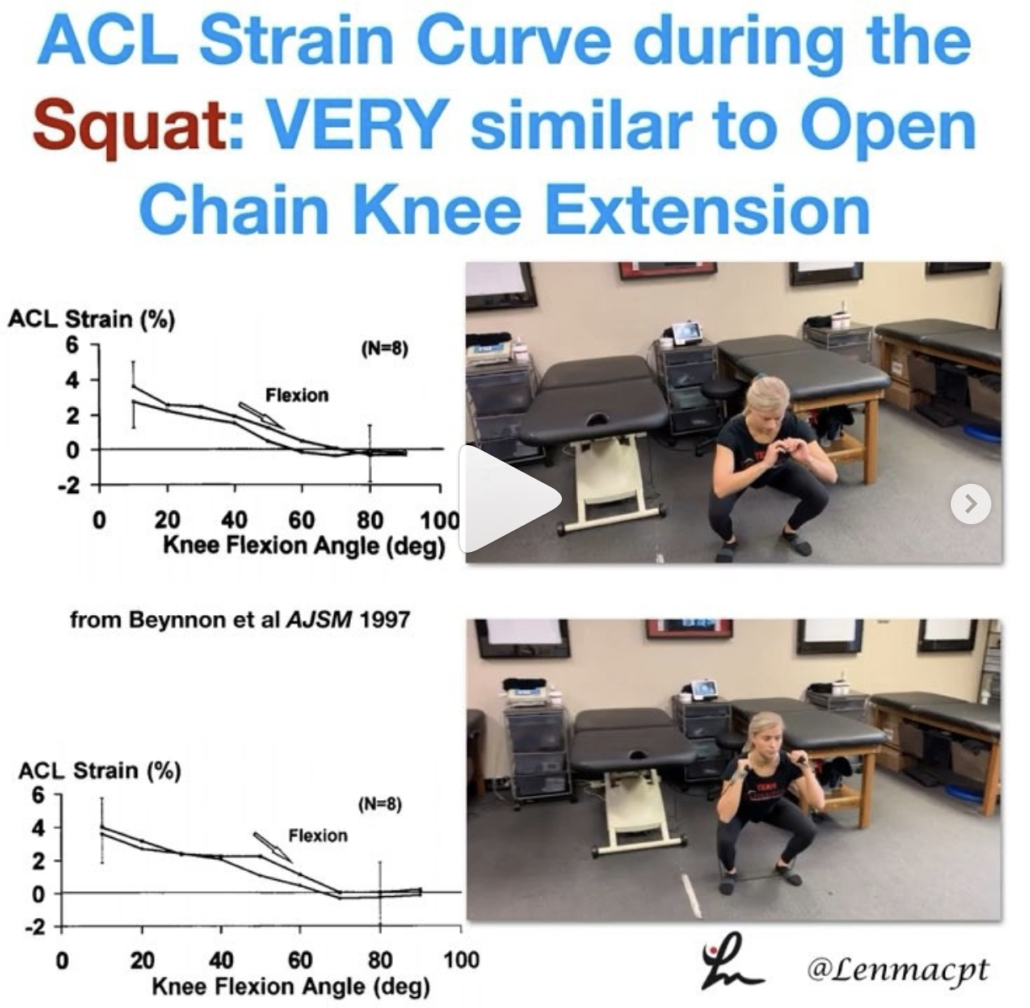
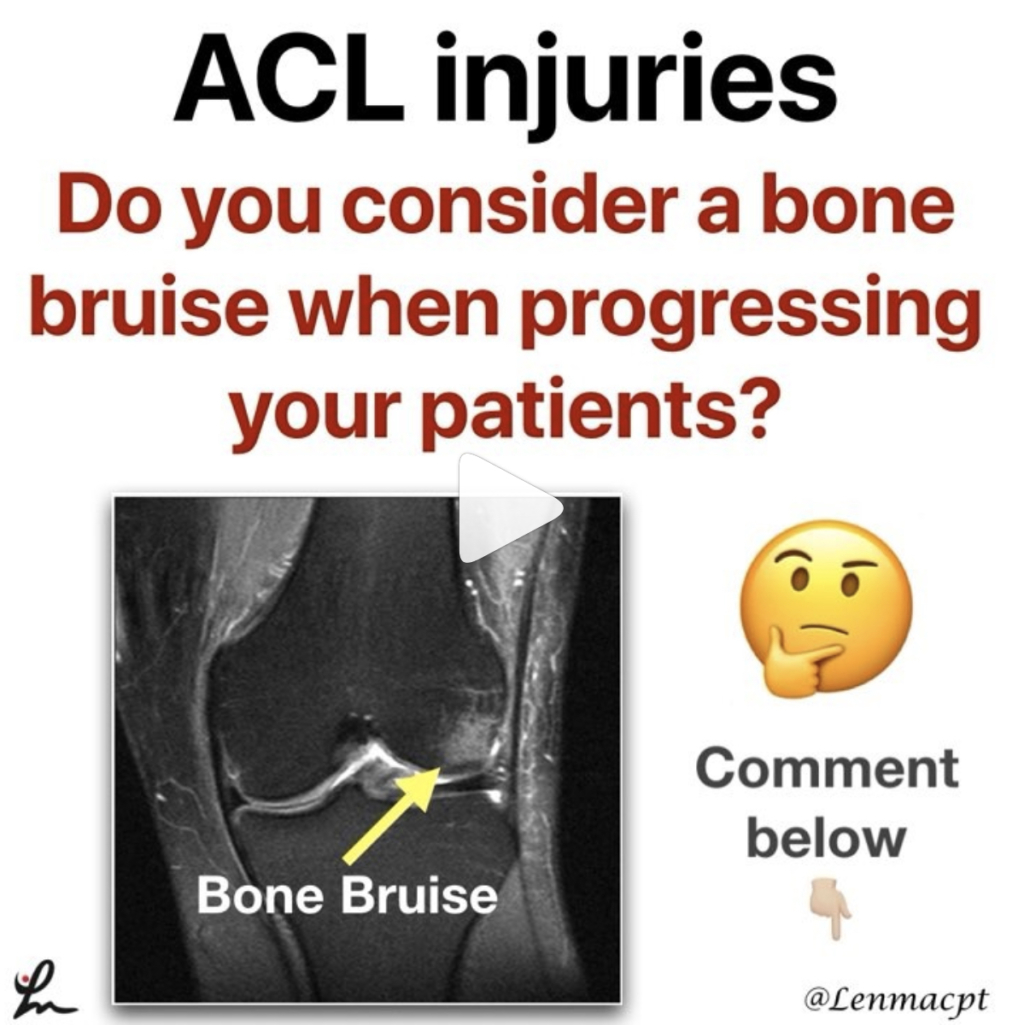
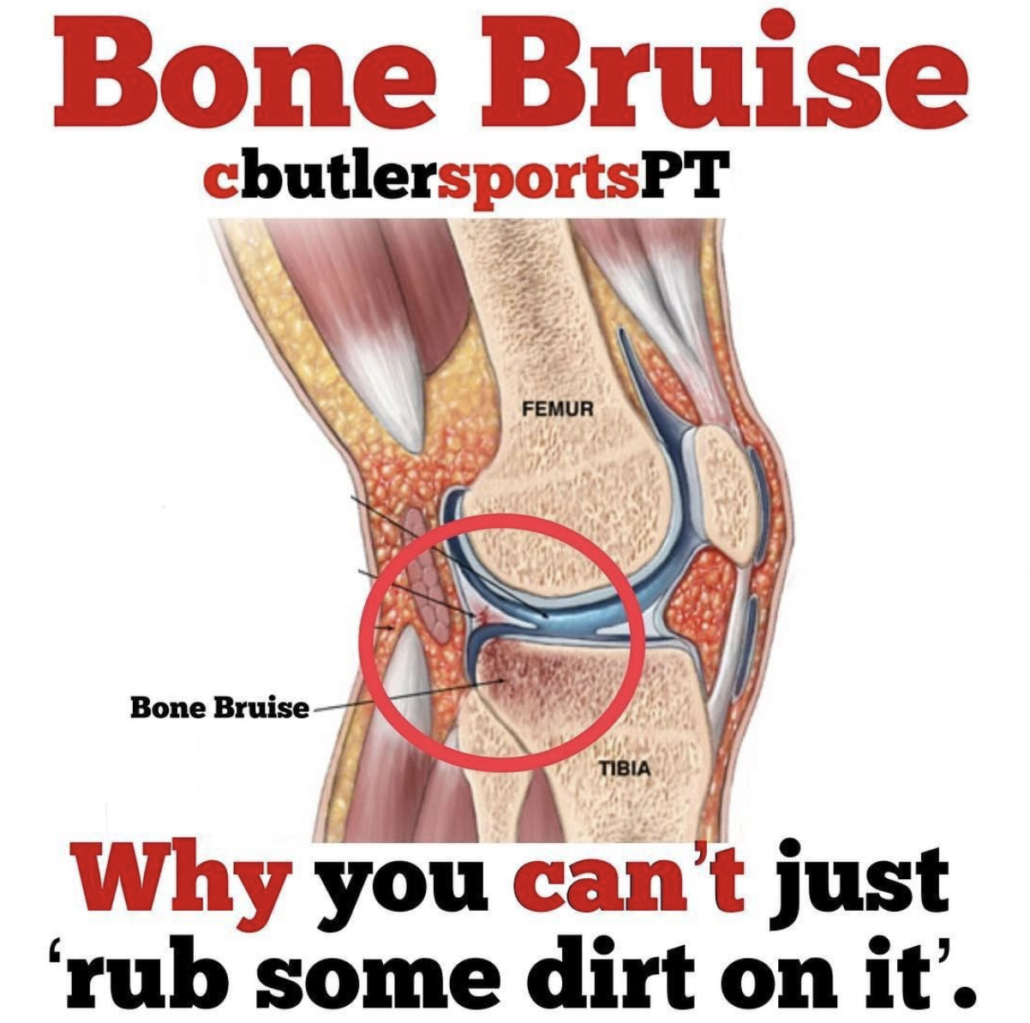
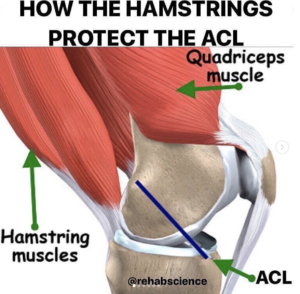
Neuromuscular training to reduce ACL injuries in female athletes
Critical components of neuromuscular training to reduce ACL injury risk in female athletes: meta-regression analysis. Sugimoto et al BJSM 2016.
This meta-regression analysis looked at the effects of combining key components in neuromuscular training (NMT) that optimize ACL injury reduction in female athletes.
They looked at a total of 14 studies that met the inclusion criteria of the current analyses. A total of 23 544 athletes were included.
They showed that there are 4 Key components
✅14-18 years old better than other age groups
✅2x/week for 30 minutes/session
✅Balance, planks, ‘posterior chain’ and plyometrics
✅Verbal cues like ‘Land softly’ or ‘Don’t let knees cave in’
Furthermore, inclusion of 1 of the 4 components in NMT could reduce ACL injury risk by 17.2–17.7% in female athletes. A great look that really specifics what age groups would best benefit from a NMT program. Do you incorporate any of these key concepts into your programs, even 1-2 of them?
I know I try to with most of my clients, whether or not they’re returning from an ACL or not.
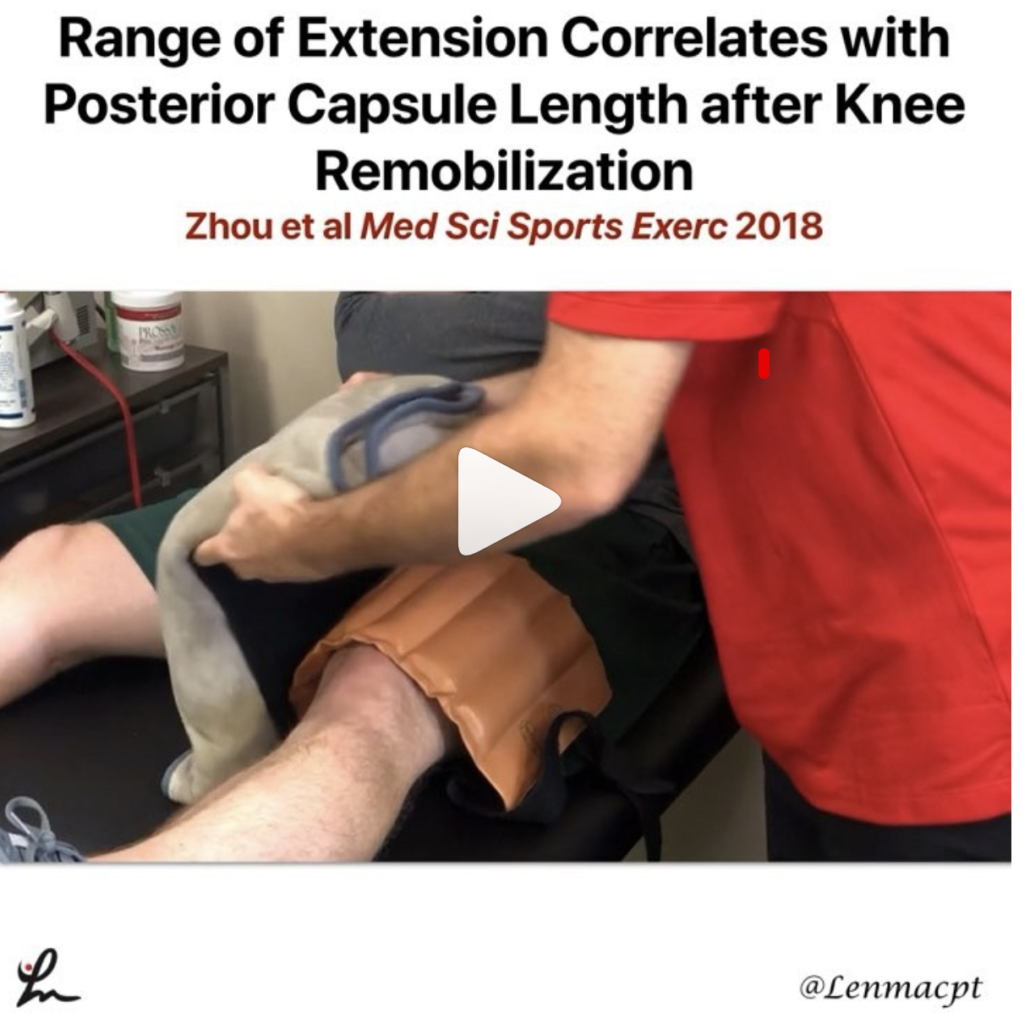
Patella mobility during a knee scope
Great video by @physionetwork looking at the patella during a knee scope. This stuff is just exciting to see (in my opinion) because it gives us a little bit of insight into what is exactly going on during a patella mobilization.
In my opinion, the PF joint is often overlooked when it comes to knee surgery and it can affect joint mechanics, quadriceps activation and patient function. You need to mobilize the patella and normalize the motion…can’t stress this enough!
Check out the post below…good stuff!
Patellar mobilization is important to avoid stiffness after surgery. In this video, you can see from an arthroscopic view that little motion outside the knee, translates into a significant motion inside the knee. Mobilization may help prevent the formation of scar tissue and allow for better biomechanics of the knee joint.
We review the latest and most clinically relevant research in physiotherapy. Click link in bio to learn more and boost your knowledge 🔗
Video by Jorge Chahla, MD, PhD – Orthopaedic Surgeon -Sports Medicine Specialist
Active Reposition Drill after a Passive Motion
Loss of proprioception after a shoulder injury has been documented numerous times in the literature and can affect long-term function.
This drill may help the rehab specialist to test proprioception by measuring the exact active position difference that the patient attains.
You can also use this drill as a treatment reproduce the exact position that you passively brought them into.
Give it a shot and see what you think…you can use this drill for any joint in which you have assessed proprioception loss.