Treating Patients with Low Back Pain
My thoughts on treating low back pain
As many of you may know, I have been practicing physical therapy since 2003. Throughout that time, the clear majority of my patients have had injuries to their extremities. Yet, I somehow was able to ‘avoid’ treating patients with low back pain (LBP). As has been with most of my career, I wanted to share my thoughts on treating low back pain and how I went from completely confused, to utterly intimidated and finally to embracing a common injury.
My early years of LBP rehab and confusion
When I first graduated from PT school, I worked in an outpatient sports medicine practice in North Carolina. I saw a little of everything. There, I was mentored by a very senior PT who specialized in low back pain.
She tried to introduce me to the rotated innominate (didn’t even know what that meant at the time) and how she could fix people with those issues. I looked at the charts of her patients and they had been coming for years.
To me, that seemed like they trusted her and she was helping them. Then I realized quickly that maybe there was more to the story. Maybe she was or wasn’t helping them, but I could never say anything. Something was working so this new grad just went with it.
She would spend hours of her time explaining the pelvis and how we could influence its position. My mind just couldn’t grasp the biomechanics. To this day, I think I’ve blocked out many of the concepts because they just didn’t make sense to me.
They even sent me to an Institute of Physical Art class out in western NC. Again, I couldn’t grasp it which is ironic because I’m very much a biomechanics type guy when it comes to the extremities.
The back was just a mystery to me!
Nothing against the IPA course, but it didn’t jive with me. I just couldn’t apply it to my patients when I didn’t understand it in the 1st place.
Going back to my rotated innominate… I just faked it that I could feel the sacral torsion or the elevated ASIS.
As a new grad, I didn’t want to seem like my palpation skills sucked so I went along with the process. I just never applied it to my patients. I just did exercise with them, because that’s all I knew.
The Evolution of my LBP Fear
When I moved to HealthSouth in Birmingham, AL we had a separate spine department that was run by 2 PT’s. You know what that meant, I didn’t treat any spine patients!! Not sure why they did that, but I wasn’t going to complain.
This trend continued on when HealthSouth had a little accounting issue and Champion Sports Medicine was founded in late 2004.
Again, no spine patients on my schedule for ~ 10 years. Rarely, a patient would be on my schedule for more than a visit or 2 before I’d move them to the “Spine PT.”
Spine Scaries
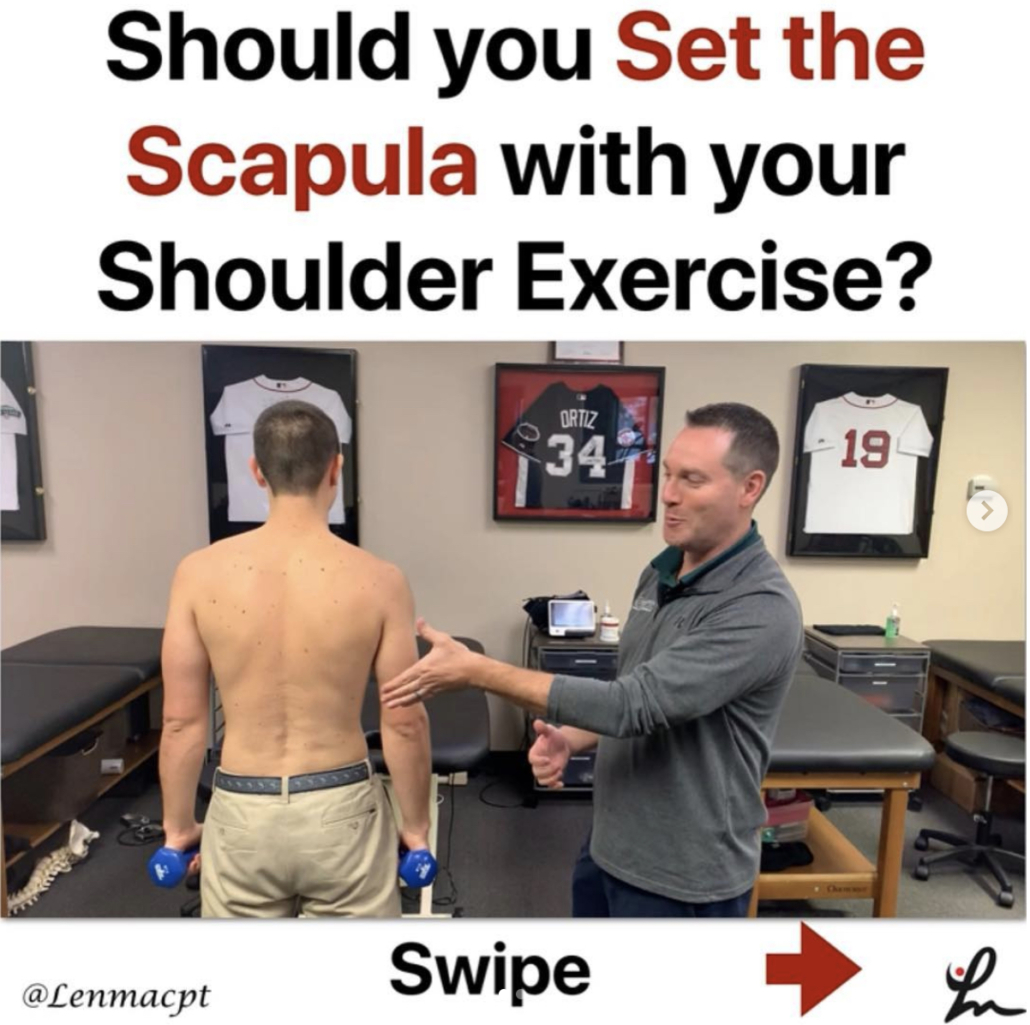
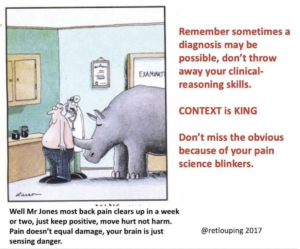
I just didn’t have an interest in the spine and from what I had seen and heard, I didn’t agree with many of the ‘theories’ out there. I watched other PT’s look for limitations in individual spinal segments from the cervical spine to the sacrum…and even the coccyx (mind blown!).
Any time someone tried to teach me their assessments, I could never feel what they were feeling. No one felt limited or rotated unless I pushed a little harder with one thumb, then all of them were ‘rotated.’ I’m right handed so everyone seemed left rotated because I could push harder into the patient’s anatomy with my right hand.
So again, my faith in spine rehab dwindled and I built my practice around sports medicine and post-op injuries. That’s my niche but I knew that when I moved to Boston to help open Champion PT and Performance that I would have to make my skills better.
My current Approach to low back rehab
My career has been about simplifying my approach to physical therapy. In my earlier days, people were trying to help me (definitely grateful) but conceptually I just couldn’t grasp it.
I knew that there were very small the joints in the spine, but I just couldn’t ‘feel’ the millimeter or 2 of motion that was present. My palpation skills were dismal, but it turns out we may not be able to palpate what we think we’re palpating. (research) (More research) (even more research)
With that, I needed a game plan for my big return to my hometown, Boston.
My Macro Views
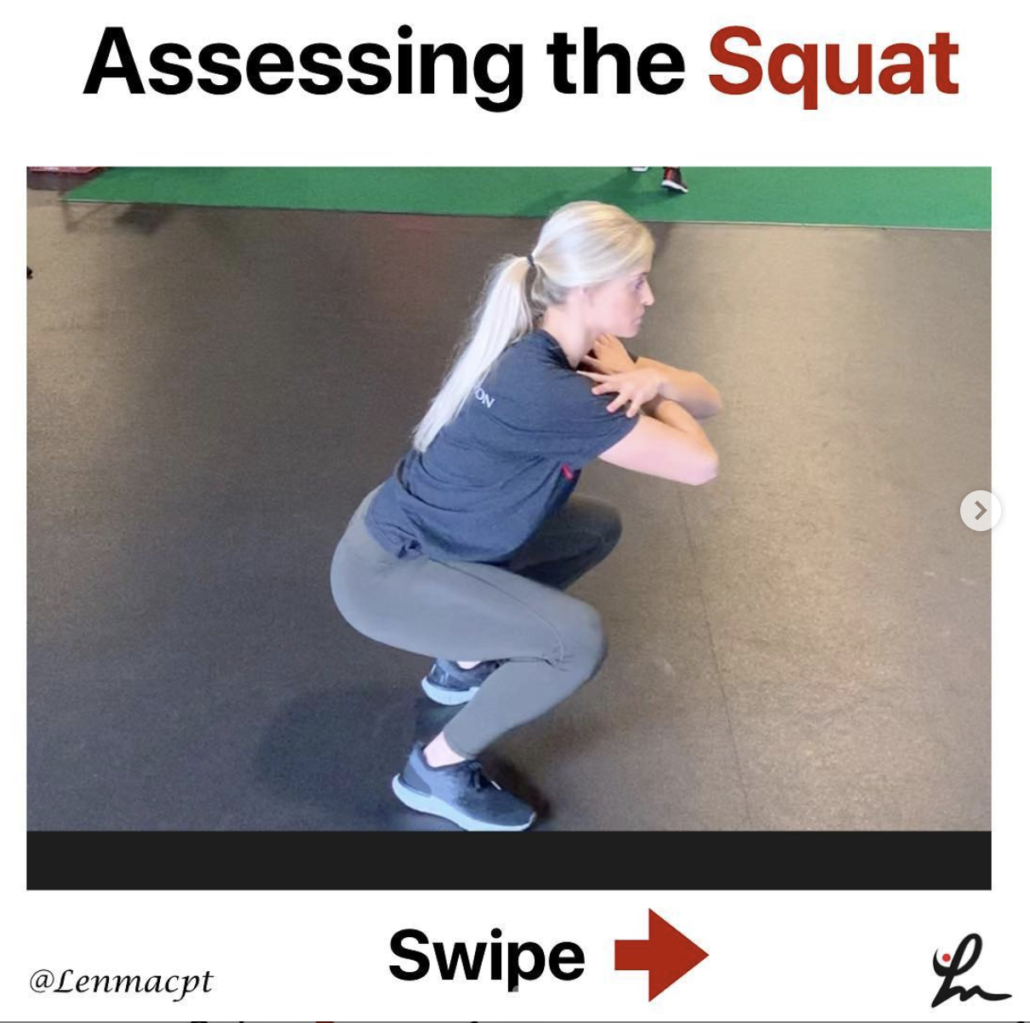
In my head, I could conceptualize watching someone move and trying to figure out if a movement dysfunction was the culprit. More of a macro view of the person instead of a micro view, like looking at individual joint segments.
My macro approach often came back to a strength issue or a simple overuse issue that led to back pain. We often blow this off and don’t account for it in our education and treatment.
Don’t Overcomplicate it!
In PT, we try too hard to complicate things.
Let’s think about it, if someone has pushed their tissues beyond their physiological limits (whatever that means), then something has to give.
In my opinion, most people that I see have overuse injuries as a result of overactivity or inactivity. It’s that simple. They’ve either pushed their muscles/joints beyond their capacity and the body is giving a warning.
Or they just don’t do enough to maintain, and the body is pissed off.
Answer in the details
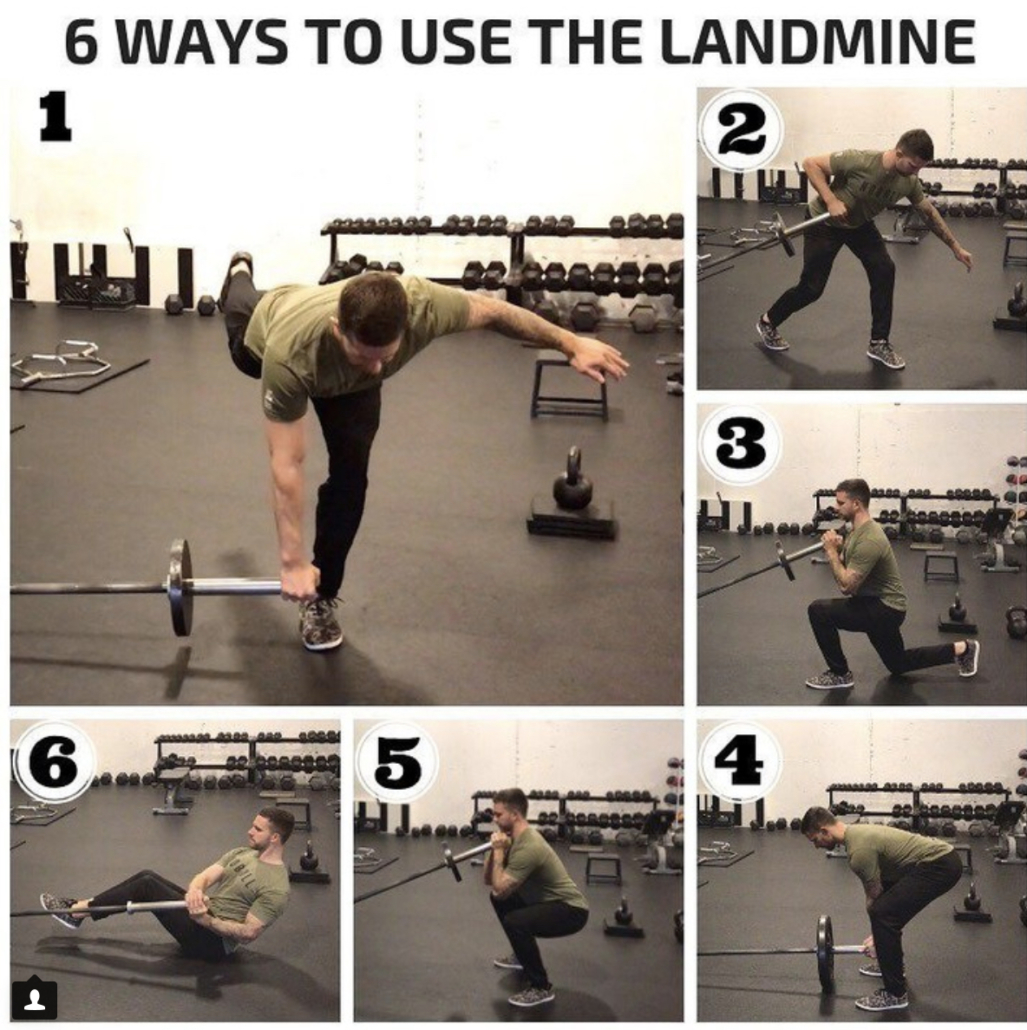
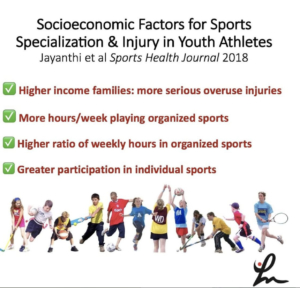
For example, I see many people with non-specific low back pain that are active. Either playing baseball or working out. But, when you dive a bit deeper into their lives, they may have just started a new program that had more volume (weight training volume, more swings of the bat, more deadlifts).
It’s often stories of their (in)activities that are directly contributing to their current state. Never mind if you dive even deeper, then they reveal a stressor in their lives that MAY also be adding to their pain.
I am certainly not a pain science expert, but I can add up 1+1 and realize that life stress + physical stress can play a HUGE role in someone’s experiences of pain.
How I treat Low back pain
So what I do is pretty simple.
I assure my patients with lots of education and encourage early motions. Like any other joint, our body needs to move. Our joints need to move.
The last thing I want to do is discourage someone from moving.
I need to create an environment that is relatively pain-free and creates confidence in their ability to move. Trust me, I’ve been there!
What helped me, you ask?
I had an acute low back spasm a few years ago that was awful!
Advil, foam rolling my low back (what seemed to be my quadratus lumborum), soft tissue work to my low back (again, maybe my QL) and general low back/hip muscles and exercises. No one told me that I had a rotated innominate or that I had too much motion at L5/S1.
I don’t even know what that means.
All I did was try to move each day with a little less pain. I did things like Cat-Cow and dead bugs. I also did clams and bridging. I stretched my hip flexors and tried to squat a bit. I just did anything to promote a safe and pain-free movement.
It built confidence and it built function.
Most people need that after they hurt their back. I know we’re always looking for the reason why the pain occurs. We try to blame the anatomy or the biomechanics because we’re ‘movement experts’.
Keep it Simple
But I say we need to take a step back and realize that it can be even simpler than that. If we sit 8 hours a day, then we’re stagnant and our tissue capacity dwindles. Imagine sitting all day then randomly try to go play 18 holes of golf!
The muscles, tendons, ligaments and anything else in that area are not conditioned for the 90+ strokes it will take to finish the frustrating round.
You wouldn’t try to run a 10K without training for it 1st. Your legs and the cardiovascular system just wouldn’t allow it.
It’s the same thing with the concept of sitting all day then trying to be active. It often won’t work. You need to train the tissue!
Final Thoughts on Low Back Pain
If anything comes out of this blog, I hope it takes some of the scary thoughts that are out there and simplifies them a bit. The human anatomy is so much more complicated than we think. We can’t just blame a rotated innominate or left rotated lumbar spine segment for the dysfunction.
All of the systems seem to play a role but as PT’s we think we can control a couple of them.
I say build tissue capacity by a general strength training program that builds confidence in the client. Let them leave feeling super positive about themselves and I guarantee that your outcomes will be so much better.
No worrying about fake palpation, popping backs and charts that are years deep of short term relief. Hope I didn’t offend anyone but sometimes the truth hurts and I want my readers to hear my simple perspectives.
Now get out there and embrace your next low back pain patient (but don’t worry about the cavitation!)