Is Early Physical Therapy Safe After a Rotator Cuff Repair?
Physical therapy is vital after a rotator cuff repair and continues to be common in an outpatient setting. Unfortunately, there’s no true consensus on when to actually begin PT. Is early physical therapy safe after a rotator cuff repair or should we delay PT to protect the healing tendons?
Let’s dive into this and see what the research is saying…
Why I’m writing this post on rotator cuff rehabilitation
It seems as if we’re all over the place despite the research, which is pretty typical. Some docs prefer early passive range of motion (PROM) while others wait 6-8 weeks (and even up to 12+ weeks for a revision repair) before they allow any form of PT.
For the record, I’m going into this blog post as a firm believer of early PROM. It’s what we’d been doing for years in Birmingham at Champion Sports Medicine.
It’s what I only knew until I moved to Boston in 2014. Now I’ve seen a nearly 180-degree turn in rehab thoughts. Much more conservative!
I recently got in a Twitter discussion (debate) about this same topic with some very respected and prominent PT’s in the field.
It made me think about things so I decided to do a little research to see what the literature says. You can check out the discussion here.
Twitter can be confusing and tough to follow but just trust me, it goes on for a while!
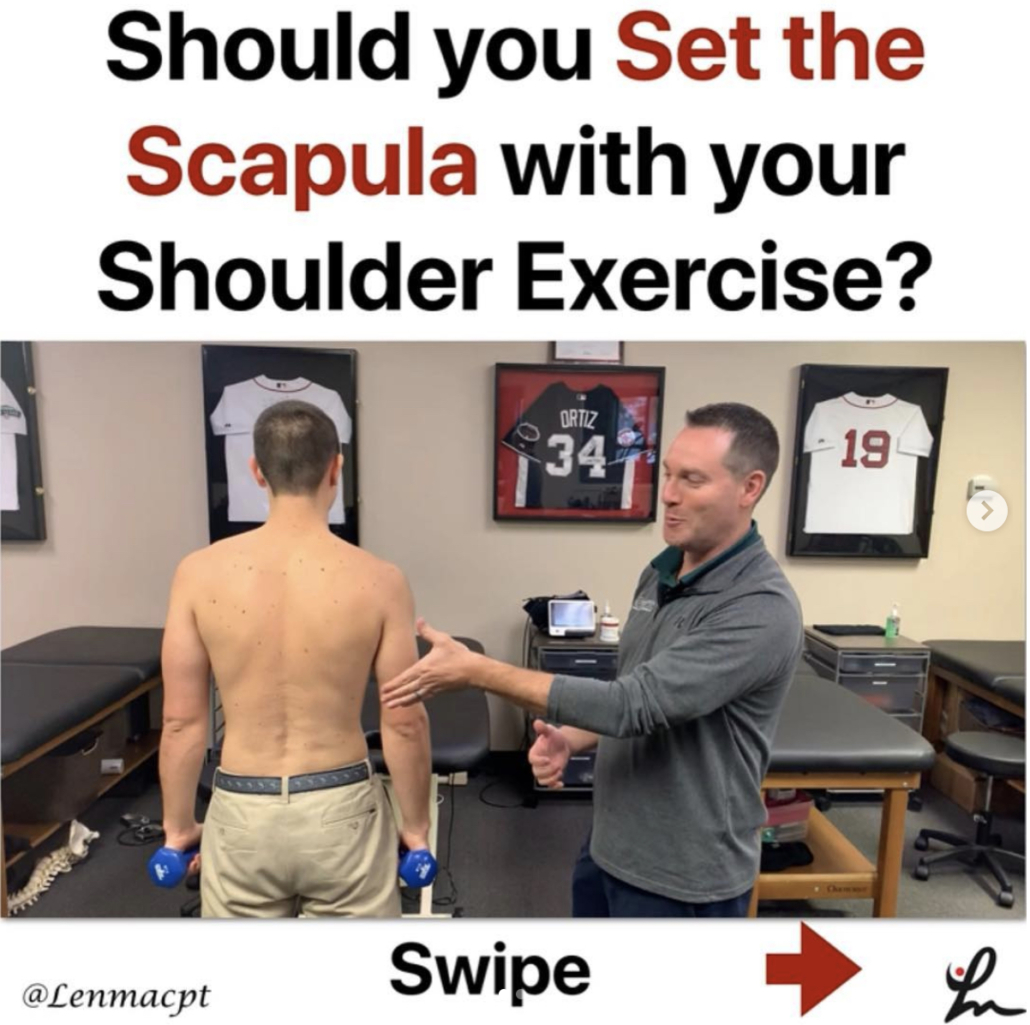
Rotator Cuff Anatomy
The tendon most commonly torn is the supraspinatus tendon. Don’t get me wrong, you can tear the other rotator cuff tendons (infraspinatus, teres minor, subscapularis).
Keep in mind a medium, large or massive rotator cuff tear often will involve the infraspinatus tendon. If it does, then you need to consider modifying your progression appropriately.
But for the sake of this post, I’m going to stick to an isolated supraspinatus tendon for now.
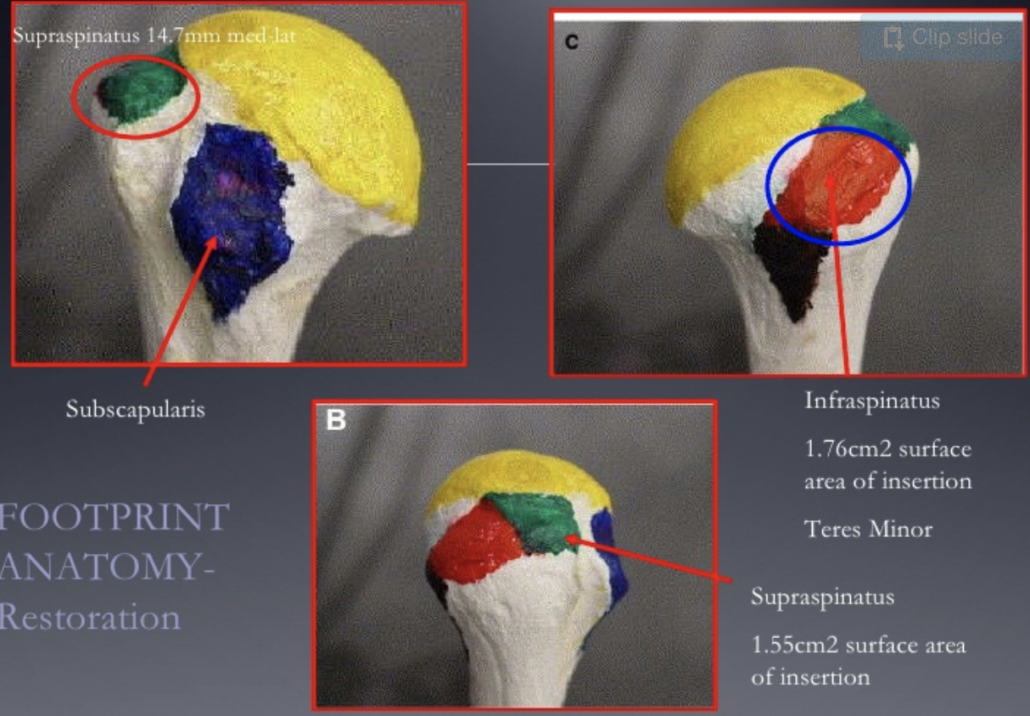
Rotator Cuff Tendon Size and Location
Look at the size of the tendons as they insert on the greater tuberosity. You’ll see it differentiated by antero-posterior and medial-lateral directions.
According to my colleague and friend Jeff Dugas out of Birmingham, he showed in 2002 that the mean dimensions of the supraspinatus insertion were 1.27 cm in the medial-to-lateral direction. For the anterior-to-posterior direction, the supraspinatus dimension was 1.63 cm.
It helps to know this information because you may need to read an operative report and see the size of the tear. The docs will usually mention a 2 cm tear or something like that.
That means that the supraspinatus tendon and a small portion of the infraspinatus tendon were involved (and repaired.)
This is critical information to have when you’re trying to plot the post-op rehab progressions and determine the prognosis. The more tendons involved, then the higher the chance of repair failure.
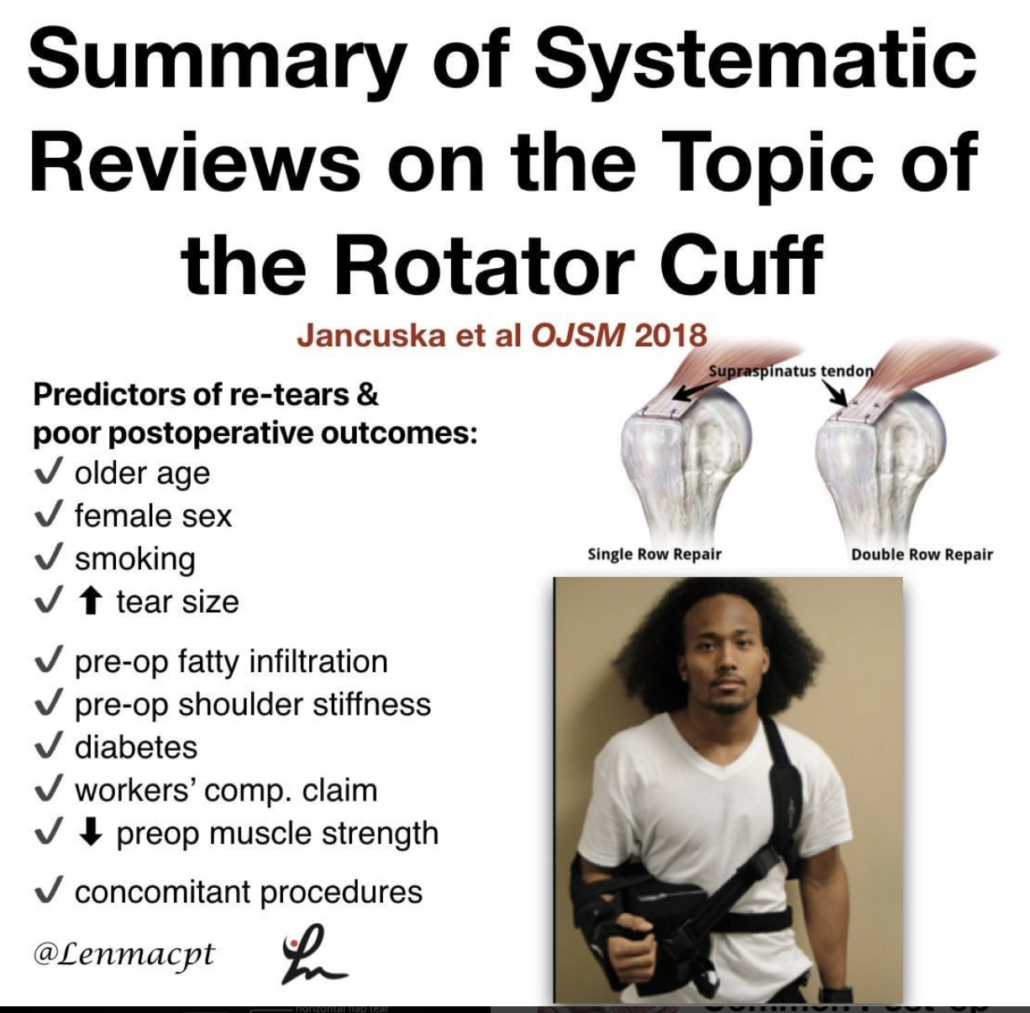
There are many other factors that influence retear rates but tendon repair size is definitely one to consider.
Rotator Cuff Repair Surgery Types
I’m not going to bore you with the details of a repaired rotator cuff. There are numerous surgical techniques being used by orthopaedic surgeons.
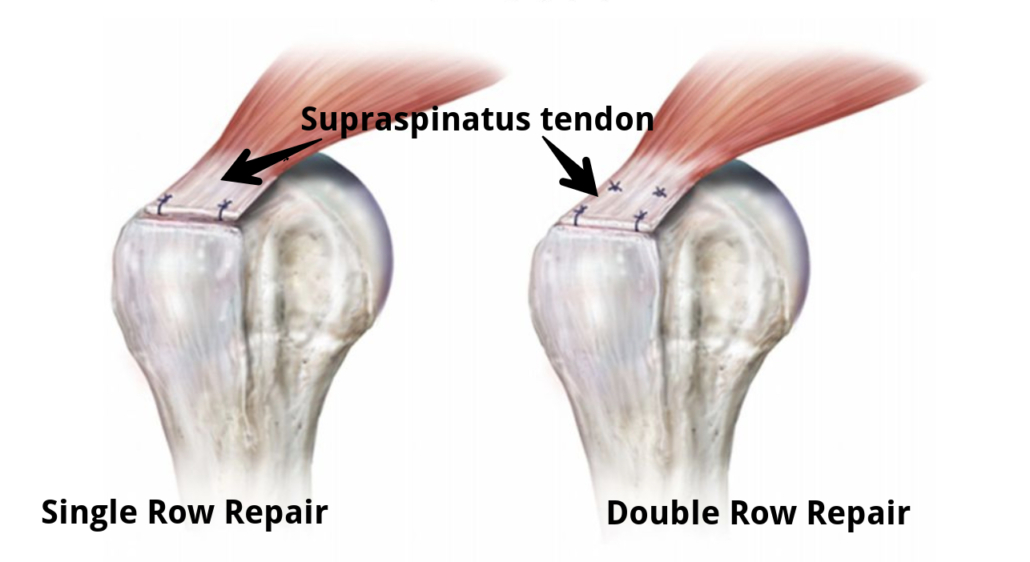
Techniques such as a single row, double row, suture bridge or transosseous repairs are commonly performed. The picture below shows the difference between a single row and a double row repair, for example.
As you can see below, the double row tends to repair more of the tissue back to the humeral insertion point, which in theory has led to better tendon healing. This has been shown in numerous research studies and has become the best technique available.
So you had shoulder surgery…when to start physical therapy?
That seems to be the million dollar question! The research is all over the place. This means that doctors’ opinions are all over the place too, right?
Keep in mind that I’ve written about this in the past. Rotator cuff repair surgery is not always warranted and can be avoided!
Since I joined the group in Birmingham in 2002 (as a PT student), we had our post-op rotator cuff repair patients starting PT post-op day 1. They started PT early regardless of the tear size. This means a small tear of 1 cm in length started PT the same time a massive, 5 cm repair would start PT.
Some may disagree with this start time but it worked…it just worked. At least I think!
Why Early PT after a Rotator Cuff Repair
This is Key!!
There were several reasons why I think it worked:
- They could chat with a professional
. - Patients better understand their pain and get reassurance that what they were feeling was normal.
- Someone could monitor their incisions and answer any and all questions
. Begin early, gentle ROM which often helps with pain control, too.
But, that was our ‘protocol’ and it continues to be that way many years later. Most other doctors that I have dealt with outside of Birmingham have taken a far more conservative approach to post-op rehab.
Agree to Disagree
Here in Boston, most docs wait at least 2-3 weeks and even up to 8-12 weeks to begin PT. Talk about eye-opening!
I don’t agree with this premise and wanted to dive a bit deeper into the literature to see if early physical therapy had a detrimental effect on short-term, mid-term and long-term outcomes.
Structure vs Function
The problem that continues to plague the research is the measurement of outcomes. Doctors care about the structural integrity of their rotator cuff repair. They see the research and are concerned with retear rates that hover in the 25-70%+ stratosphere. Of course I’d be concerned with retear rates that high!
Can you imagine if ACL re-tear rates were that high? Well, guess what they still hover in the 6-40% range even with our tremendous rehab skills and return to play testing.
But fortunately, we have other parameters to consider with our patients after a rotator cuff repair. We can look at the pain-free function!
Huh, what a novel idea. Regardless of the integrity of the repair, many patients can still live their lives to the fullest and in most cases without any pain.
Start PT Early after a Rotator Cuff Repair? What does the literature say…
I’m going to do my best and unbiased research to figure out if early PT after a rotator cuff repair is safe and effective compared to a delayed protocol. Let’s take a look…
There are a bunch of studies out there that you need to sift through. You can tell when the lead authors are MD’s or PT’s because the docs want to make sure their repair integrity is intact and the PT’s are concerned with restoring ROM, strength, and function.
With that, I’ve done my best to pull out some studies that have helped guide my practice and continue to influence me today.
Literature Review Findings
Age a BIG Factor!
Mind you, Cho et al showed that healing rates after a rotator cuff repair drastically change for older patients compared to younger patients.
The slide below was taken from my rotator cuff lecture that I’ve done in the past and helps to put things in perspective.

In no particular order…
Parsons et al JSES 2010 looked at 43 full thickness RTC repairs who were in a sling for 6 weeks. All were without PT for that time then evaluated for stiffness in PROM. They defined stiffness as 100° flexion/ 30° ER.
Overall, of the 43 surgeries, 23% (n=10) became stiff after that 1st evaluation session. The whole cohort displayed a 56% retear rate overall at 1 year, which to me seems crazy high!
To break it down further there was:
- 30% retear in stiff group
- 64% retear in non-stiff group
- There was no significant difference in ROM or functional scores.
In my opinion, there were some pretty big limitations to the study that should be exposed, like:
- Single row repair
- No consideration for Diabetes or smoking
- MRI without contrast to re-evaluate the repair status
- What is “ER by the side???”- need to better define what degree of abduction.
So getting stiff may be a good thing but the repairs were done as single row repairs. We know these did not heal as well as they do with double row repairs.
More Literature Reviews
Moving on to a 2014 Level II systematic review and Meta-analysis, the authors said “the results contradicted our hypothesis that immobilization would increase tendon healing compared with an early-motion rehabilitation protocol, as structural outcomes were similar in the two groups 1 year after the arthroscopic repair of rotator cuff tears.
From the paper: “We speculate that rehabilitation is not the sole factor affecting tendon–bone recovery; the effects of other factors, such as older age, fatty degeneration, larger tears, and surgical technique, may outweigh those of the rehabilitation protocol.”
Kim et al AJSM 2012 looked at small to medium sized RTC repairs. They compared immediate PROM (0-120 degrees) to 4 weeks of absolute immobilization. They eventually showed no difference in ROM, pain or tendon healing. So seems like a smaller tear of less than 3 cm may be appropriate for immediate ROM, albeit it was limited to 120 degrees for some reason.
Not sure why they limited to 120 degrees because it seems as if the tendon would shorten as the humerus is placed in further flexion. Maybe they were concerned with subacromial impingement or something but the limitation is a bit confusing to me.
Healing Affected?
Another study by Lee et al AJSM 2012 wanted to compare ROM and healing rates between 2 different rehabilitation protocols after arthroscopic single-row repair (use caution) for full-thickness rotator cuff tear.
They showed pain, ROM, muscle strength, and function all significantly improved after arthroscopic rotator cuff repair, regardless of early postoperative rehabilitation protocols.
They also looked at the repair integrity with postoperative MRI scans, 7 of 30 cases (23.3%) in the immediate ROM group and 3 of 34 cases (8.8%) in the delayed group had re-tears, but the difference was not statistically significant (P = .106).
Well then, only a trend and all had similar functional outcomes regardless of when they started ROM…I’d say that helps the case to start early.
But again, these repairs were done via a single row repair and they allowed manual therapy 2 times per day and unlimited self-passive stretching exercise, which seems a bit aggressive anyway.
Do we even need a sling for 6 weeks?
No Functional Difference Between Three and Six Weeks of Immobilization After Arthroscopic Rotator Cuff Repair: A Prospective Randomized Controlled Non-Inferiority Trial Arthroscopy 2018
This study looked to compare clinical and radiologic results among patients with 3 versus 6 weeks of immobilization after arthroscopic rotator cuff repair in a prospective randomized controlled non-inferiority trial.
They concluded that “3 weeks of postoperative immobilization with sling use was non-inferior to the commonly used regimen involving 6 weeks of immobilization in a brace.” For the structurally concerned people out there, MRI indicated similar degrees of healing between the groups.
Well then, that throws a wrench in things for the docs!
Does Early vs Delayed PT Affect Outcomes?
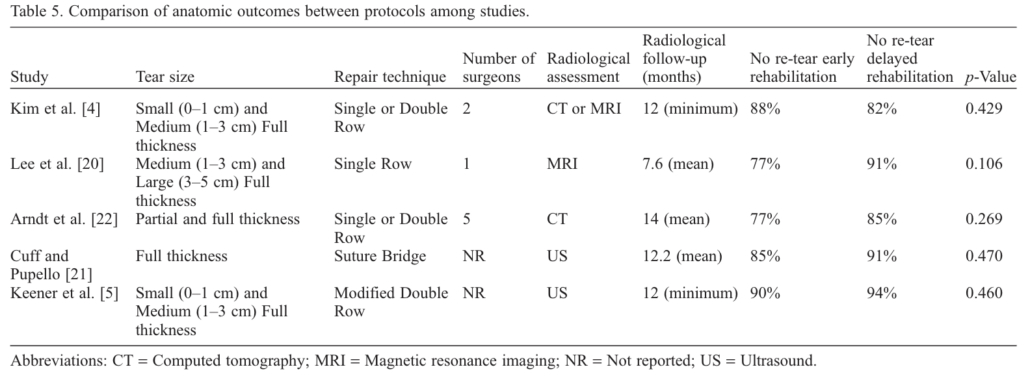
A systematic review by Gallagher et al 2015 looked to determine if there are differences between early and delayed rehabilitation after arthroscopic rotator cuff repair in terms of clinical outcomes and healing. Six articles matched their criteria and reported significantly increased functional scores within the first 3-6 months with early rehabilitation compared to the delayed group.
To me, this is huge! Put yourself in their position. Imagine feeling better and being able to get back to work a little quicker. That’s my major argument for starting rehab sooner. Earlier pain relief, improved function and a feeling of being normal again.
Furthermore, none of the included studies reported any significant difference in rates of rotator cuff re-tear.
Medium-Large Tears use Caution
However, two studies noted a trend towards increased re-tear with early rehabilitation that did not reach significance. This was more pronounced in studies including medium-large tears. A similar trend that I’ve seen in the literature.
Here’s a nice table from that Gallagher study that summarized their findings for each research paper they included:
I want my patients to feel good as quick as possible and get back to some semblance of a normal life. But of course I want the long-term integrity of the repair to remain intact. And it seems as if this study helps that argument.
Then you look at a group of PT’s from Turkey (Duzgun et al Acta Orthop Traumatol Turc. 2011) that looked to compare the effects of the slow and accelerated protocols on pain and functional activity level after arthroscopic rotator cuff repair. Patients were randomized in two groups: the accelerated protocol group (n=13) and slow protocol group (n=16).
There was no significant difference between the slow and accelerated protocols with regard to pain at rest.
The accelerated protocol was superior to the slow protocol in terms of functional activity level, as determined by DASH at weeks 8, 12, and 16 after surgery.
I’ll take that!
Function over Structure (at times!)
Told you that the PT groups tend to favor function over structure, haha!
Early passive Motion ok- The French Version
This next study out of France that included French Society for Shoulder & Elbow (Orthop Traumatol Surg Res. 2012) looked to compare the clinical results after two types of postoperative management: immediate passive motion versus immobilization. Patients were randomized to receive postoperative management of immediate passive motion or strict immobilization for 6 weeks.
They concluded that their results suggested that early passive motion should be authorized: the functional results were better with no significant difference in healing. Functional results were statistically better after immediate passive motion and a lower rate of adhesive capsulitis and complex regional pain syndrome.
Seems as if there may be a trend but certainly not an overwhelming conclusion that early ROM is guaranteed to lead to inferior structural results. But, it seems pretty conclusive that ROM, pain, and function are improved after early ROM.
Let’s continue to look at the research
This group from China (Shen et al Arch Orthop Trauma Surg. 2014 Sep) performed a systematic review and meta-analysis to determine whether immobilization after arthroscopic rotator cuff repair improved tendon healing compared with early passive motion. Three RCTs examining 265 patients were included but we need to be cautious because of the limited number of studies included and the heterogeneity of the samples.
They found that there ‘no evidence that immobilization after arthroscopic rotator cuff repair was superior to early-motion rehabilitation in terms of tendon healing or clinical outcome. Patients in the early motion group may recover ROM more rapidly.’
This recent 2017 study in the Journal of Shoulder and Elbow Surgery included 9 meta-analyses in its review. They basically
They also concluded that “Whereas early motion and delayed motion after cuff repair may lead to comparable functional outcomes and retear rates, concern exists that early motion may result in greater retear rates, particularly with larger tear sizes.”
So, it seems as if function and healing the same after a RTC repair but there may be a discrepancy once we start looking at a larger repair size.
Immediate PT after a Revision Rotator Cuff Surgery
This study in AJSM 2018 looked to evaluate the clinical and radiological outcomes after revision rotator cuff repair surgery. They were able to track 31 of 40 patients (77.5%) for the final assessment at a mean follow-up of mean 50.3 months.
Interestingly enough, physical therapy started on the first postoperative day with passive flexion and abduction.
Revision rotator cuff repair improves clinical outcomes and shoulder function at midterm follow-up. The clinical outcome scores were comparable in patients with an intact repair and those with failed RC healing.
And they started PT 1 day after the surgery and got PT 2-3 times per week.
Retear Rates and Long-term function
This study in JBJS 2006 looked to determine the clinical and structural outcomes of re-ruptures in twenty patients after a longer period of follow-up. Nineteen of the twenty patients continued to be either very satisfied or satisfied with the outcome.
At an average of 7.6 years, the clinical outcomes after structural failure of rotator cuff repairs remained significantly improved over the preoperative state in terms of pain, function, strength, and patient satisfaction.
They also found that re-ruptures of the supraspinatus that had been smaller than 400 mm(2) had the potential to heal….wow!
Failure Rates too High!
Another study in JBJS 2013 looked at 18 patients who had undergone arthroscopic repair of massive rotator cuff tears. At two years of follow-up, 94% had a failed repair. This current study wanted to evaluate the 10-year results for these patients with known structural failures of rotator cuff repairs.
Despite a high rate of progression of radiographic signs associated with large rotator cuff tears (proximal humeral migration or cuff tear arthropathy), most did well.
Clinical improvements and pain relief after arthroscopic rotator cuff repair of large and massive tears are durable at the time of long-term (10 years) follow-up. They went on to say:
“These results demonstrate that healing of large rotator cuff tears is not critical for long-term satisfactory clinical results in older patients.”
So our obsession with healing rates still appears to be overblown, even in older patients with a known cuff tear.
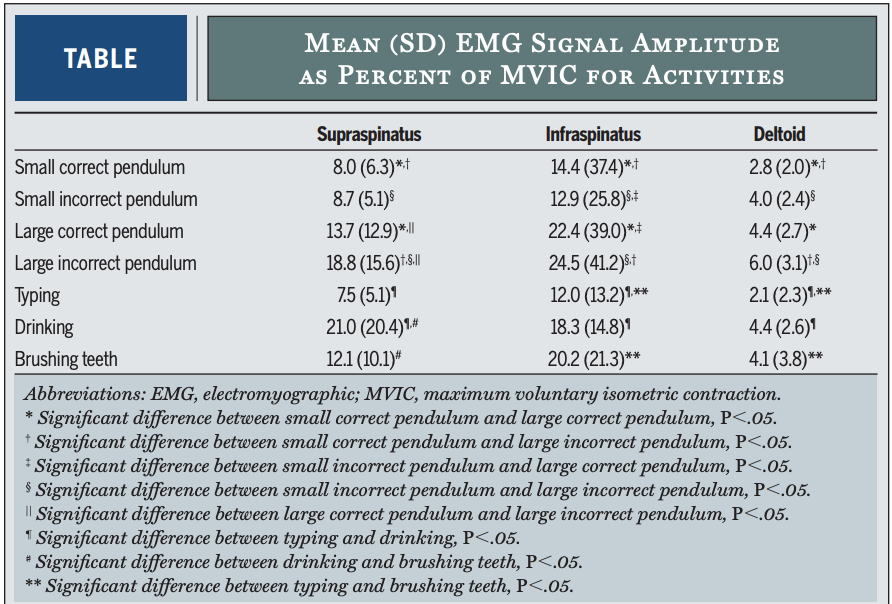
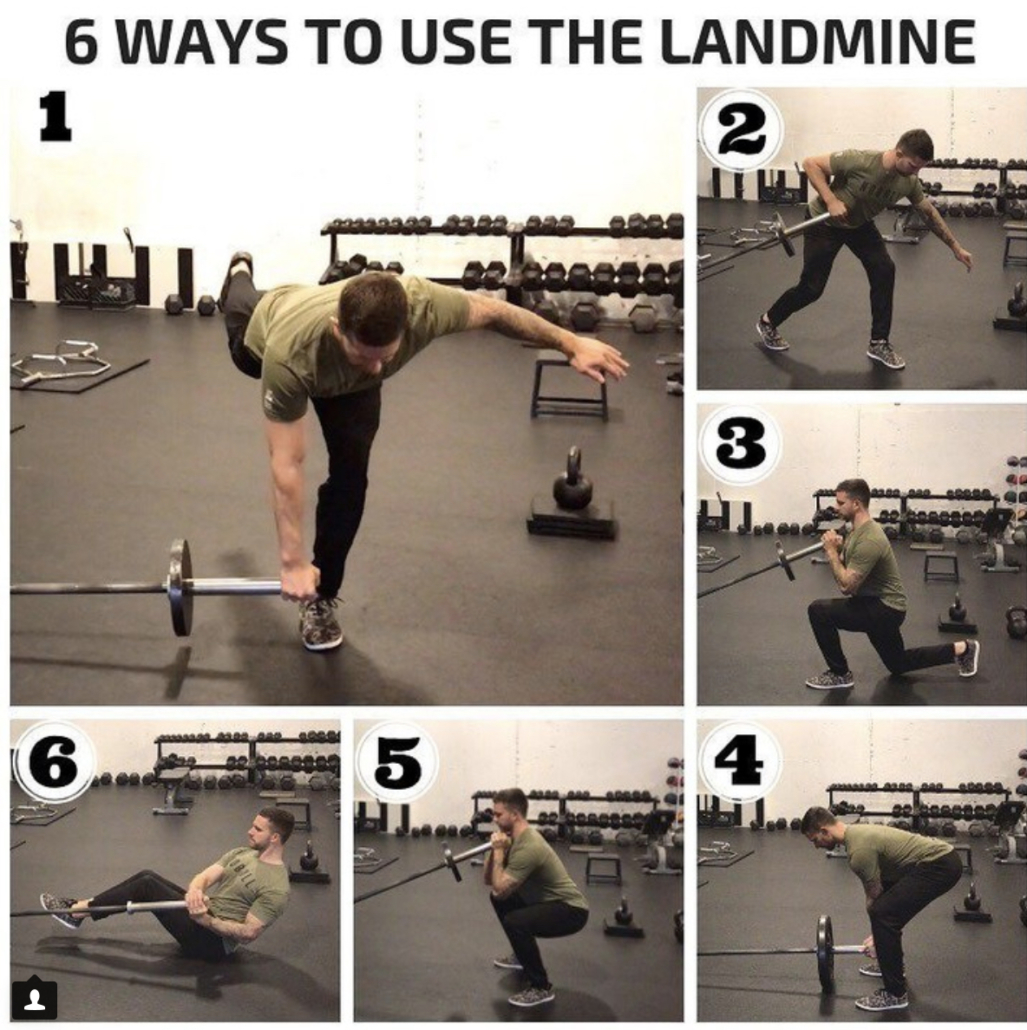
Pendulum Exercises Effects on Muscle Activity
Activation of the Shoulder Musculature During Pendulum Exercises and Light Activities JOSPT 2010
Look at that Paper in JOSPT 2010 (I’ve pulled out the Results Table for you below).
If there’s one exercise that doctors allow after a rotator cuff repair then it’s a pendulum or Codman exercise. How often does our patient do them correctly and make it a completely passive motion? I’d say rarely if seldom, right?
Most often, the patient is just bent over and actively moving their shoulder. They have no body movement or sway. Most of the movement is shoulder based and are not completely relaxing their shoulders.
Furthermore, they were instructed in the doctor’s office that 1st week or 2 after surgery.
They’ve been doing them incorrectly for weeks on end because they have no one to help them (cough cough!)
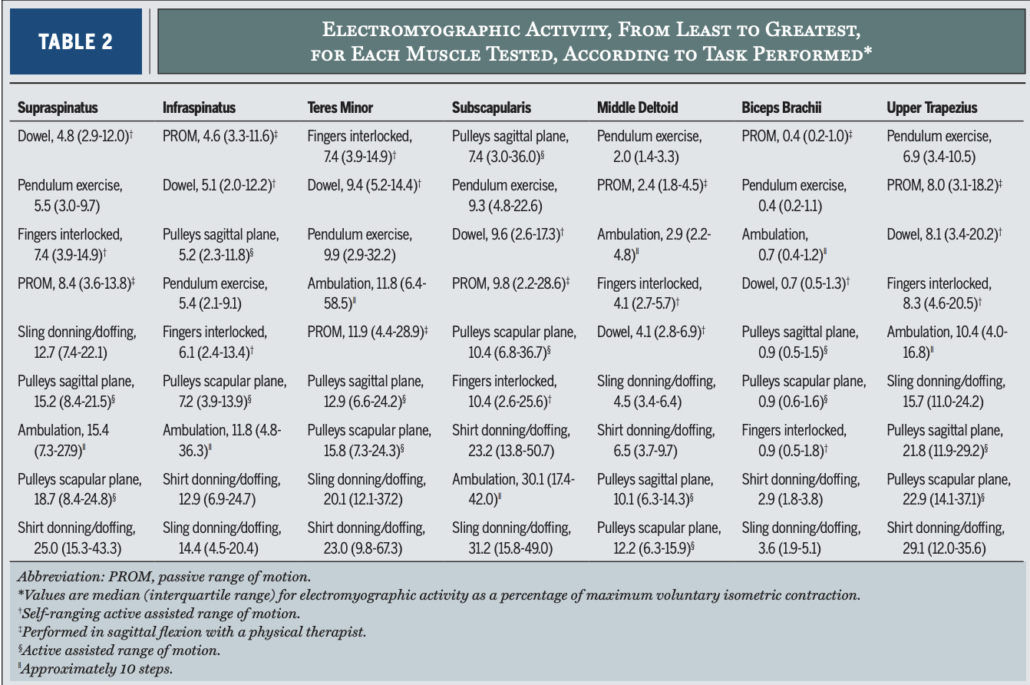
EMG of common Rehab ExerciSES
A study in JOSPT 2016 looked at EMG activity in healthy individuals. They wanted to quantify muscular activity during daily tasks and common PT motions. They showed that “of all the tasks assessed, ambulation without a sling and donning and doffing a sling and a shirt consistently showed the highest activity.”
EMG results table is found below.
Pretty helpful to see it listed by muscle and EMG activity and specific movement.
EMG of contralateral movements
A pretty neat EMG paper from 2004 (small n=6 and healthy individuals) were assessed using fine wire and surface EMG during common functional activities of the contralateral extremity while immobilized.
They found high supraspinatus EMG activity of the immobilized shoulder for all fast pulling activities of the contralateral shoulder (25-32%)!
Furthermore, they found high infraspinatus activity (56%) of the immobilized shoulder when the contralateral extremity performed straight forward reaching activities.
So even if they are immobilized and using their non-operative shoulder for daily activities, the rotator cuff is still sustaining a higher amount of activity than anything that we would do in the early phases (PROM, dowel self-ROM, rope and pulleys, properly performed pendulums).
How about revision rotator cuff repairs, you ask?
This study from AJSM in 2018 looked at outcomes after a revision rotator cuff repair. They showed revision rotator cuff repair improved outcomes regardless of tendon integrity (MRI confirmed).
Oh boy, what is going on??
Dig deeper into the study and they started PT the 1st day post-op with passive flexion and abduction. Sounds familiar, no? And this was in revision surgeries.
We used a very similar approach in Birmingham as they did in this study, so I may be a bit biased.
My Closing Thoughts on Physical Therapy after Rotator cuff repair surgery
I think it just shows you that rehab can begin early, will not affect long-term outcomes and that tendon integrity is not correlated to function.
I honestly don’t think our 15-30 minutes of passive motion early on in the rehab process is significantly affecting outcomes and retear rates.
It seems as if the repair technique, contralateral arm daily use, compliance with proper exercises (like pendulums, for example).
Let’s not blame early PT. There are so many more variables that are more likely to affect rotator cuff repair outcomes than anything that we could do in PT.
So I say let’s get people into PT early, educate them, guide them and help them get over this painful surgery.
I’ve been doing this for years and have seen the benefits of early PT. I say the literature agrees with me!