This week’s articles discuss a wide variety of research topics. We discussed:
- Risk Factors for ACL tears
- Injury after a concussion
- EMG of the hip to minimize TFL activity
- We made of our posture and applied it to daily tasks
- Rhythmic Stabilization drills for the shoulder
Hope you enjoy and make sure to share with your friends and colleagues!
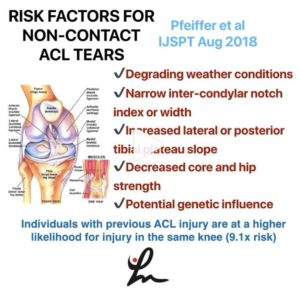
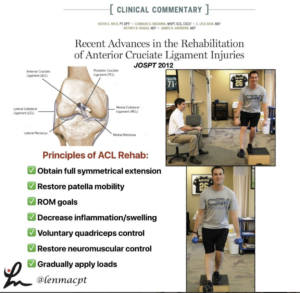
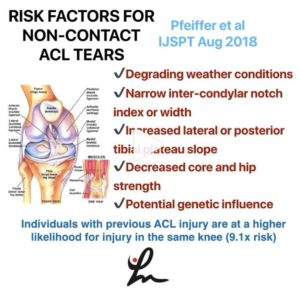
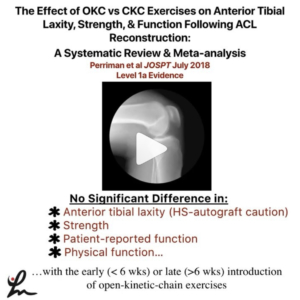
Factors Associated with Non-Contact Anterior Cruciate Ligament Injury: A Systematic Review. Pfeiffer et al IJSPT Aug 2018
This study looks to examine the existing literature for risk factors associated with non-contact anterior cruciate ligament (ACL) injury in both sexes.
A total of 79 full-text articles were reviewed, 55 of which met criteria for inclusion.
✔️Degrading weather conditions⠀
✔️Narrow inter-condylar notch index or width⠀
✔️Increased lateral or posterior tibial plateau slope⠀
✔️Decreased core and hip strength⠀
✔️Potential genetic influence
Individuals with previous ACL injury are at a higher likelihood for injury in the same knee (9.1x risk).
Take a look at this study because they do a good job of breaking down the literature and pointing out some of the common risk factors, both extrinsic and intrinsic.
✅Anatomic factors⠀
✅Neuromuscular Factors⠀
✅Physiologic Factors⠀
✅Biomechanical Factors⠀
✅Genetic Factors
Check out this paper and tag a friend or colleague that may benefit from reading this paper.
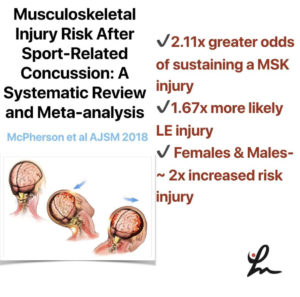
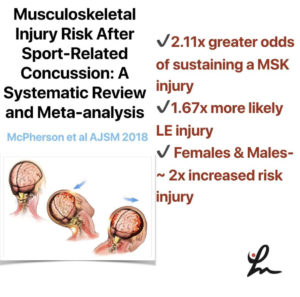
Musculoskeletal Injury Risk After Sport-Related Concussion: A Systematic Review and Meta-analysis – McPherson et al AJSM 2018
This systematic review & meta-analysis looked to determine the odds that athletes will sustain a musculoskeletal injury after a concussion. It was hypothesized that a concussion would increase the risk for MSK injury.
Eight studies met inclusion criteria for meta-analysis reporting 860 male and 163 female athletes with concussion compared with 3719 male and 507 female control athletes without a concussion.
✅Athletes with concussion had 2.11 times greater odds of sustaining a MSK injury compared with control groups and 1.67 times more likely to experience a lower extremity injury.
✅Female athletes with concussion had 2 times greater odds to sustain injury compared with non-concussed female control athletes.
✅Male athletes with concussion similarly demonstrated an increased odds of 2.1x risk for injury compared with non-concussed male control athletes.
Of course, they say further studies are needed to determine the physiological reasoning behind the increased risk for injury after a concussion.
Kinda makes sense, right? Anecdotally I feel like we see this a lot but good to be able to see it in the literature and educate our clients prior to a return to their sport.
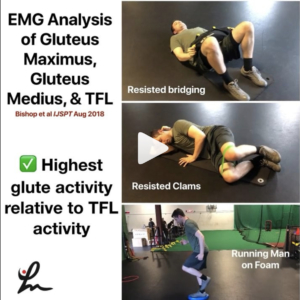
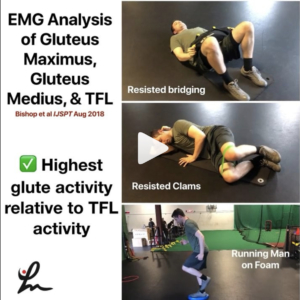
Electromyographic Analysis of Gluteus Maximus, Gluteus Medius, and Tensor Fascia Latae During Therapeutic Exercises With and Without Elastic Resistance. Bishop et al IJSPT 2018
This study looked to determine the gluteal-to-tensor fascia latae muscle activation (GTA index) and to compare electromyographic muscle activation of the GMax, GMed, and TFL while performing 13 commonly prescribed exercises designed to target the GMax and GMed.
Clams with and without resistance, running man gluteus maximus exercise on the stability trainer, and bridge with resistance, generated the highest GTA index respectively.
It seems as if these 3 exercises may give you the biggest bang for your buck when trying to maximize gluteal activity and minimize TFL activity.
Knowing previous research, it seems as if most single-leg-stance exercises are going to give the patient the best gluteal activity per EMG.
Do you guys use any of these exercises? Maybe you need to use them more for your patients looking to improve their hip strength.
Tag a friend who may need bigger 🍑 and may benefit from this research by the esteemed Barton Bishop and his research team! TThanks, carlokoo for modeling!⠀

Loss of knee extension after a surgery can greatly impact a patient’s function in the long term.
Although opinions vary greatly in the orthopaedic world, I am a firm believer that regaining symmetrical knee extension is critical for a surgery to be successful.
Shelbourne et al showed that the number one factor in determining long-term satisfaction after a knee surgery was symmetrical knee hyperextension.
Per Benner et al 2016, obtaining full hyperextension that is anatomically normal for most patients does not affect objective stability, ACL graft tear/failure rates, or subjective scores after ACL reconstruction with patellar tendon autograft.
So why do some docs and PT’s still think you only need 0 degrees of knee extension? 🤔⠀
I’m not sure but I’ll tell you it is safe to get hyperextension and here are 3 tools that I use to help regain that last bit of motion.
1. Low load long duration in supine: in my opinion a better position to regain extension and more comfortable than hanging a patient’s leg off of a table. You try doing that and see how you like it!
2. Retro treadmill walking: walking at ~ 1.0 mph on the treadmill has been a great way to get that last bit of motion back and is something they can do at their gym when they’re not with you in PT.
3. Retro cone walking: Again, the goal is to accentuate the end range into hyperextension and it will also challenge their dynamic balance.
So, do you use these techniques with your patients? If not, tag a friend or colleague that may benefit from seeing this post!
I love when we can make fun of ourselves & this post nails it! Give @beardthebestyoucanbe a follow!
There is no such thing as good or bad form or posture. There is no right or wrong “exercise”. What does “functional exercise” even mean, & what is this “core” thing everyone keeps talking about whilst planking or crunching?! My newsfeed is blowing up with these so-called “fitness coaches” and “rehab experts” putting all type of crap out there. For 1 of 2 reasons, maybe both⠀
1. Pure ignorance⠀
2. Trying to grow their following by giving people what they think they want⠀
_⠀
The only bad posture is the posture we spend too much time in (shout-out Andreo Spina). Life is not perfect posture & neither is sports⠀
As human beings, our movement capacity should be vast. If we only stay in a small handful of postures we aren’t fulfilling our movement potential and we’re creating more dysfunctions and weaknesses because of it. Your body will devolve rapidly⠀
If you always hammer down the same posture, even if it’s “good posture”, you’re only creating strength and neurological control in that specific posture. So when your body slips out of that particular shape, weakness and injury is the outcome – and that’s not a good sign⠀
There is no such thing as a functional exercise, just functional (or non-functional) joints that can fulfill movement potential. If your joints can’t successfully control a range of motion that is necessary for your daily life, you should probably make that a priority for your training practice⠀
So in conclusion, is it that you need to practice good form (and never lose it, ever)…or practice multiple forms⠀
How do we practice in those ways? Well, it’s going to take a philosophical change first and foremost. Understanding our biology and neurology is important⠀
If you do not know how to train in such ways, find those who do.
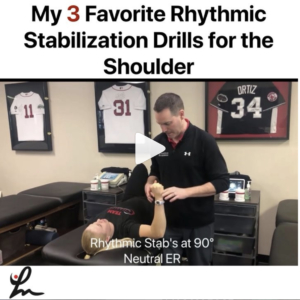
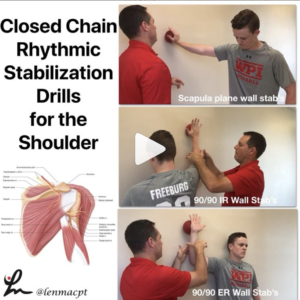
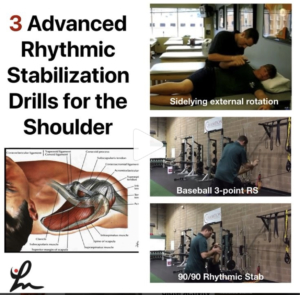
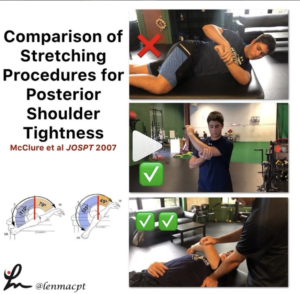
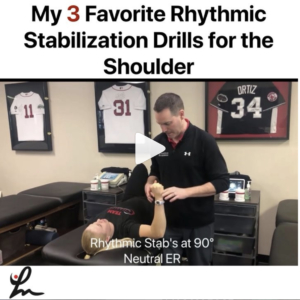
I use Rhythmic Stabilization drills daily in my practice for most of my upper body patients.
I think they are critical to use to help the patient regain neuromuscular control, a sense of their joint and it’s a great way for the PT to get a sense of how the patient is doing overall.
The hands-on strength training (trying not to trigger dependency by the patient, so relax!) is a great way to gauge a patient’s progress.
Various tools can be used to progress and regress these exercises. I hope these few basic RS drills can give you a basic understanding of what we do @championptp
I hope to get more of these videos out in the future.
Share with your friends and colleagues so they can see these valuable drills for the shoulder joint!