Lumbar Spine Stress Injuries in Baseball Players
Low back pain can be very debilitating in an athlete, especially in an adolescent baseball player trying to make it through his season. More specifically, I have noticed an increase in lumbar spine stress fractures in baseball players and it is quite disturbing and frustrating!
I wanted to dive deep into this rabbit hole, as I always do. Low back pain is way too common in youth athletes. I wanted to know why it’s happening so often and try to figure out a solution for my clients.
It can get complicated so I will try to simplify the process.
My goals:
- What is a stress fracture or a stress reaction?
- How common is this injury in youth sports compared to other sports and age groups?
- What is the typical clinical presentation?
- What are some clinical tests that PT’s can use in the clinic?
- Demonstrate a typical treatment of a young athlete with a low back stress injury?
- What are the expected outcomes?
Pain is Complicated
Low back pain can take on many etiologies. Pain, in and of itself, is extremely complicated and very personal.
It can manifest in different ways for each person. In this post, I want to talk about the athlete with an acute injury. Specifically, the youth and adolescent baseball player.
Many factors can contribute to someone’s pain including stress, anxiety, medical history, their environment, support system, etc.
This topic is a bit more personal because of what do on a daily basis. I see a ton of youth athletes with a variety of injuries. Plus, I was diagnosed with spondylolisthesis (bilateral fracture in the spine and some shifting of the vertebral body) while a junior in college so I’ve lived it myself!
Recently, I’ve started to see a lot more athletes with low back pain as a result of a stress reaction or fracture. It really made me wonder what was truly causing this in the 12-18 year old athlete.
Video example
As you can see in the video, the pre-injury video shows how long the pitching motion is for this athlete. His throwing arm is wrapped around his body which forces him to keep his weight back.
His arm is trailing his body significantly and he tries to make up for it by hyperextending his back. His timing is way off and his arm is not keeping up with his forwardly moving body.
You can see in the post-injury video that he is much more balanced. His arm also has better timing with his body. He is driving toward home plate with his lower body while maintaining a better upper body sequence
There are many issues going on here but you can see the significant changes that were made after the injury to help him improve his mechanics and hopefully prevent a future injury.
LUMBAR STRESS INJURIES DEFINED
Stress Reaction Defined
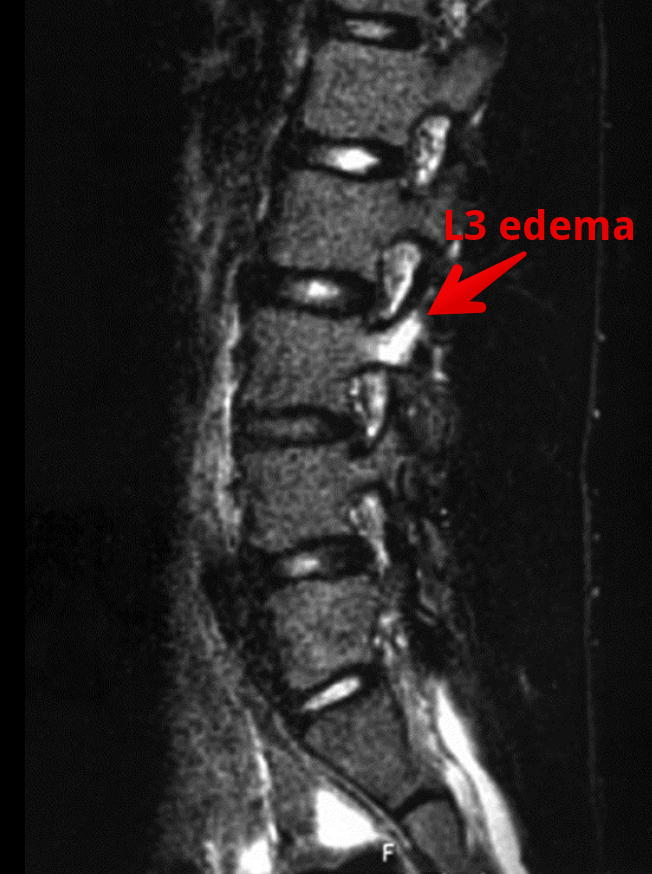
Basically, a stress reaction is the early breakdown of the bone without a clinical diagnosis of a true fracture. Often times, a suspected fracture will be diagnosed as a stress reaction. On MRI, there is only edema noted in the area and not a true fracture.
I hear a lot of people talk about fractures in different terms. Simply stated, a fracture is a crack, break, defect in the bone. Whether it’s a hairline fracture or a gross disruption of the bone may determine prognosis but the bone has been compromised.

Obviously pain is an early sign but it needs to fit the clinical presentation. Has there been a history of excessive activity or a change in the volume of playing?
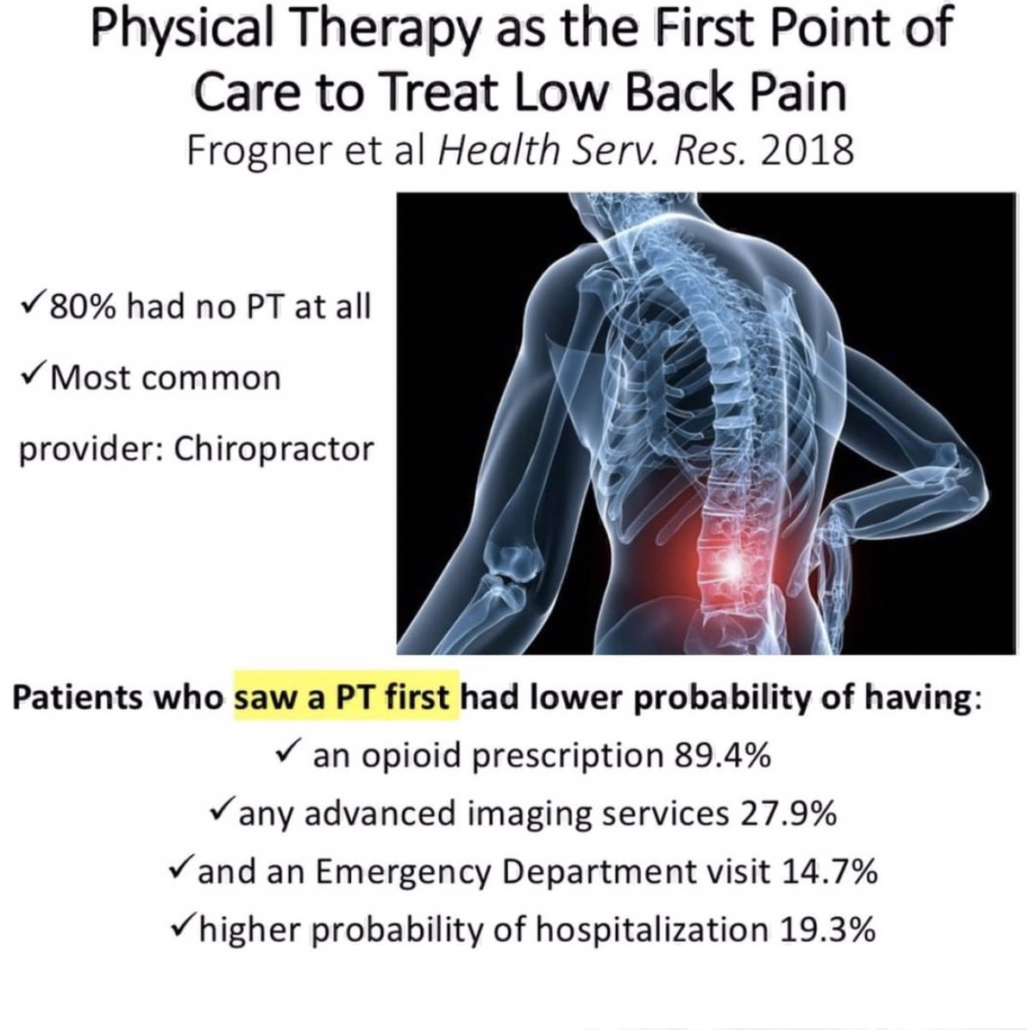
Factors to consider in a baseball player with low back pain
I usually have to dive a bit deeper into the player’s life to figure out the root cause. It’s often something very overlooked but is often the main contributor.
These are just some, off the top of my head, that may be involved in the athlete’s predicament and that may nee to be changed.
It is an early indicator that something is wrong and it can progress to a stress fracture if not carefully treated. We’ll talk treatment later on so be patient!
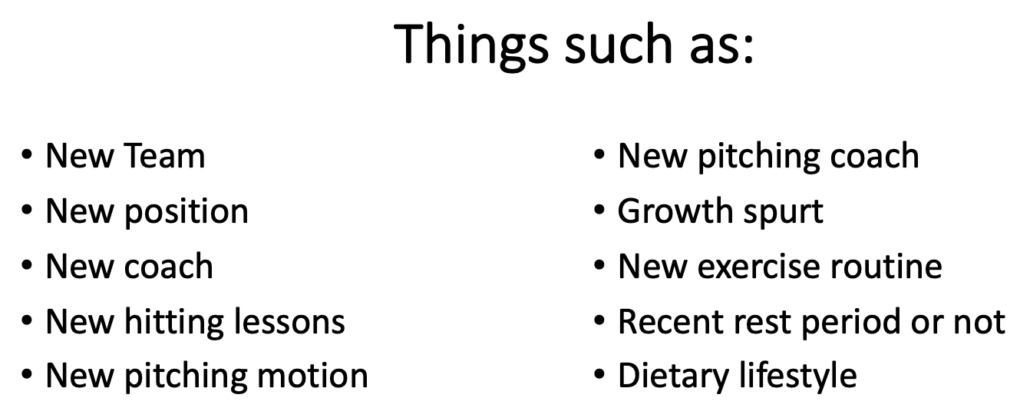
How common is a stress reaction in youth sports?
As with any research, it is quite mixed and will heavily depend on the sport that you are tracking. From what I can see, if a kid has low back pain for greater than a week, then that’s a pretty good sign that a more serious injury may be present.
For example, this retrospective case study from 2017 showed that 30% of pediatric cases with low back presenting to this hospital were diagnosed with spondylolysis.
Specializing in a single sport was not associated with an increased risk of spondylolysis when compared with multisport athletes. Male athletes were 1.5 times more likely to have a spondylolysis than female athletes.
Males with LBP who participated in baseball had the highest risk of being diagnosed with a spondylolysis, followed by soccer and hockey.
Females with LBP who participated in gymnastics had the highest risk of spondylolysis, followed by marching band and softball. I will refer to my good friend Dave Tilley and his website for his professional judgment on this one. Based on what I see at our facility, I’m not surprised.
As I usually tell my clients and their families…I’m going to treat this as a spondy until proven otherwise.
More Research on Spondylolysis Prevalence
According to recent research, it looks as if persistent pain for 1-2 weeks is associated with a positive MRI diagnosis for spondylolysis in 33-40% of the kids scanned. You can read the abstracts here and here if you’re interested in more.
This study out of New York showed that the most common athletic activities associated with spondylolysis were:
- Soccer (19.3%)
- Basketball (17.2%)
- Lacrosse (9.4%).
Of note, 71% of the children in this study were male and the most common level to have the spondy was at L5.
Do keep in mind that false positive results are pretty prevalent in patients getting an MRI for low back pain.
Don’t treat the MRI (or x-ray!)
This systematic review looked at the incidence or prevalence of incidental findings on MRI in asymptomatic pediatric patients. The results are pretty eye-opening too!
- Degenerative disc disease (prevalence 19.6%)
- Disc herniation/protrusion (prevalence 2.9%)
- disc height/narrowed disc space (prevalence 33.7%)
- Spondylolisthesis/spondylolysis (prevalence 2.3%)
- annular tear and/or nerve root compression (prevalences ranging from 4.5-51.6%)
Pretty amazing to see the prevalence of false positives read on an MRI in a pediatric population. We need to be able to clinically diagnose these first then use the MRI scan to further determine a course of action.
Baseball specific injury rates
In this study from 2015, the proportion of High School baseball players with a low back stress fracture was 3.3%. So, a typical AAU baseball club of 100 kids will have 3 kids that have a stress fracture.
They also reported that High School girls sustained more stress fractures (63.3%) than did boys (36.7%) but for overall injuries and not just in the low back. This seems consistent with what I see in my practice, as well.
In college, 12.1% of the stress fractures noted in this NCAA study from 2017 were in the low back. Women experienced stress fractures at higher rates than men, more often in the preseason, and predominantly in the foot and lower leg.
Baseball Specific low back pain
This nice review of the literature discusses low back pain in general athletes. They went on to further discuss baseball and “the asymmetric baseball postures and motions lead to asymmetric spondylosis in right and left sides and cause mechanical degeneration in intervertebral discs.”
In this study, “students who played baseball were 3.2x more likely to experience LBP in their lifetime only behind volleyball which had an odds ratio of 3.8.
The repetitive nature of the baseball specific movements and a preponderance to specialize in one sport can definitely affect these injury rates.
The role of mental stress and low back pain
The role of stress, particularly mental stress on bone development, has been studied too. Our teenage athletes are under a tremendous amount of stress at home and socially. This study from 2017 discussed the emerging concept of mental stress as an important player in bone adaptation and its potential cross-talk with physical stress.
Essentially, mental stress can have a negative impact on normal hormone production. Hormones are needed to maintain normal bone health. A shift in normal hormone regulation can negatively affect a youth’s growth and healing capabilities.
They went on to say that there is “compelling evidence has recently emerged that biochemical and psychoneuroendocrinological maladaptations caused by mental stress are not only also relevant for bone quality, but may furthermore considerably interact with physical stress.”
Clinical Presentation of a Spondylolysis or Spondylolisthesis
Clinically, pain is the guide here. It’s often described as a pretty sharp pain that is localized to the site of the injury.
There is rarely a referred pain down the leg or the buttocks. The pain is often close to the spine at the level of the injury.
In this study, activities involving repetitive hyperextension and/or extension rotation of the lumbar spine were described as painful in 98% of the patients.
Pretty powerful statement. In my examination, I look to recreate these symptoms with these exact movements.
Many use a single-legged position, also known as the Stork Test, to test for spondylosis. I’ve simplified the test to just include regular standing on 2 feet to simulate regular daily movements.
A standing extension test can also be used to assess end range extension and rotation irritability. I find this test (see video below) is a great way to begin to hone in on a diagnosis.
I find that pain in full hyperextension and rotation is a pretty powerful indicator of a stress reaction or fracture. It is similar to the standing position that I described above. However, the prone position takes the postural component out of the picture and may help to better isolate the location of the lesion.
I also like to have the patient get in the prone position and use different levels of active extension to help guide my clinical examination.
Again, people will report pain that is very close to the spine and that replicates their pain.
Any young athlete with low back pain for greater than 1 week should be assessed for some kind of bony issue in their low back.
That’s not to say that we will always find something.
But I just think that in younger athletes, this prevalence is all too common and needs to be ruled out to prevent further low back issues.
Treatment for Spondylosis in Baseball Players
Muscle tenderness too
Patients will usually have tenderness right at the region in which they have pain. I suspect it’s the muscles that stabilize those lumbar segments.
The multifidi and most likely quadratus lumborum are often implicated. Soft tissue work of any kind can have positive effects on muscle tightness. The athlete should perform some self-myofascial release with a foam roller or light pressure with a baseball in the affected muscles.
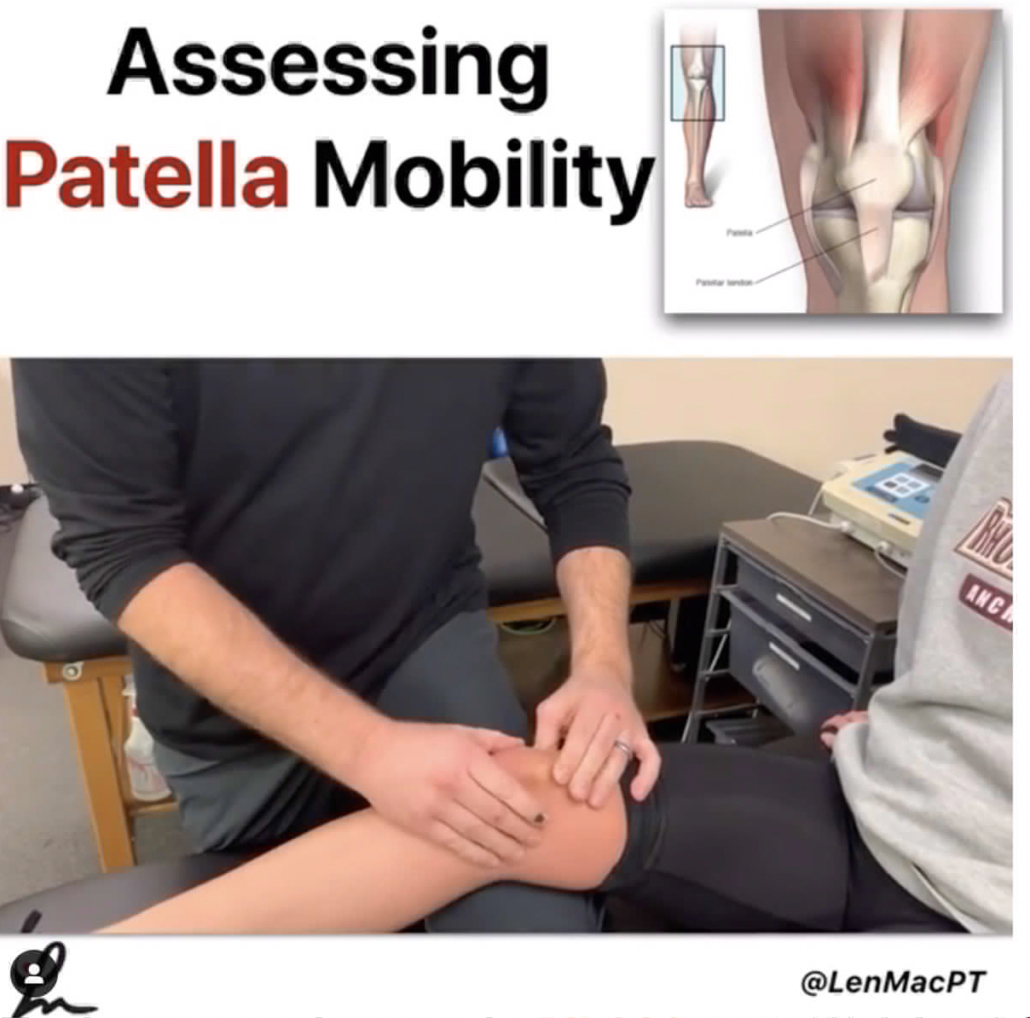
Manual therapy can also be utilized to feel tissue density and help to pinpoint the exact location of their muscle soreness. By utilizing this, I can help to better educate the athlete for their home exercise programs.
Manual Therapy can be helpful
In this photo below, you can see I am applying direct pressure with my elbow right into the muscles of the low back. The patient will usually give me feedback and tell me if I am in the right area. Muscle soreness is often detected and after a short amount of time, the symptoms should decrease.
In the short term, manual therapy can help with some of the acute symptoms. For long-term changes to occur, activity modification and exercises that involve low back, hip and core strengthening are critical.

My treatments for kids with low back pain are pretty simple. I want to rest them from the repetitive activities, such as swinging a bat or even throwing a baseball.
Brace or no brace?
Also during this time, the athlete will most likely have to wear some form of a back brace to prevent excessive lumbar extension and rotation. One particular brace is called a Boston Brace. It was developed by doctors at Children’s Hospital in Boston, MA.
The research is unclear and can favor both methods of treating with or without bracing. A study in 1986 showed that bracing ‘restricted at least some gross body motion to approximately ⅔ to ½ of no-orthosis values.’ The restrictions we’re most pronounced when wearing a larger Thoracolumbosacral orthosis (TLSO) versus just a corset.
If the goal is to restrict motion, then it seems as if a brace will accomplish that. Most research shows about 40-65% restriction in motion no matter the brace. This paper showed similar findings as well.
Here’s a version that our local docs have been using that is less cumbersome and not as embarrassing to wear as a teenager!

These are just some of my quick and easy exercises to help promote movement in the spine.
Obviously, I want to avoid painful motions like lumbar hyperextension and rotation. I still want to promote some sort of motion to build confidence and promote muscle recruitment in that area.
Specific treatment ideas for low back pain
I like foam rolling or some form of self-myofascial release to the area. This will help the muscles to feel better if done multiple times per day. See the video below
Some would say motion is lotion and I tend to agree! I like to use active range of motion through the cat-cow video below.
Some general guidelines for returning to baseball
From what I’ve seen, most baseball players need at least 3 months of active rest.
I’ve written about my general low back treatment philosophies in a previous blog post.
You can find that post here .
Active Rest is key
I generally want to begin a general strength training program at around 6-8 weeks following the diagnosis. It Is critical to include restricted range of motion exercises to avoid painful hyperextension. These exercises are restricted to avoid excessive extension that may place extra stress on the low back. I prefer to bias flexion type exercises like squats, lunges and step-ups.
I like to closely monitor their form and symptoms. We don’t want any pain at all in that region…a very important concept!
I like to perform these exercises for at least six weeks to get a good base of strength in the lower body and core.
Lose the brace at 12 weeks
At about 12 weeks, they will come out of the brace and we can begin to be a bit more aggressive in our strengthening. Again, we are avoiding hyperextension type movements in the low back. We prefer to stay in a flexed or neutral spine as much as possible.
I also like a supine dead bug exercise to promote a flexed spine with active motion. See the video below.
Throughout this time, we encourage cardiovascular exercises that involve the stationary bike. This seems to be a safe modality that allows the athlete to work up some sweat but also maintain a relatively flexed spine, which is usually pain-free.
Unrestricted activities at 5-6 months
At around 5 to 6 months post-diagnosis, we encourage for pain-free activities that involve strength training for the whole body. There are no limits in range of motion in the athlete is free to work out. We then encourage more functional activities that involve rotation. This will allow them to replicate the motions involved with hitting and throwing.
Return to sports at 6-8 months
On average, it seems as if a patient recovering from a low back stress fracture will need at least 5 to 6 months before I would feel comfortable having them return to their support. These injuries usually happen in a younger population so the risk for re-injury is pretty high if they return to their sport too quickly.
I believe the risk is high because of their underdeveloped muscular system. Their bodies are growing and tremendous stress may be placed upon their joints with excessive activities. A slow progression back to their sport is critical.
Concluding thoughts on stress fracture injuries in youth athletes
Baseball players face numerous challenges during their training.
As you can see, numerous injuries can result and not just to the shoulder and elbow.
Low back pain injuries are all too common but are often preventable. It seems as if the volume of throws and hits may play a huge role. It is up to the coach, physical therapist, or athletic trainer to monitor this workload for each athlete.
There is no exact science but listening to the athlete is critical. A well-balanced training program that addresses some of the obvious weaknesses is key.