The Week in Research Review, etc 11-26-18
This week, I discussed the progression of someone after a knee surgery. I tried to highlight the key stages and some techniques that I like to use to advance the patient’s mobility and comfort. Take a look at The Week in Research Review, etc 11-26-18 and share with your friends. Hope it helps you improve your patient care tomorrow and beyond!
ACL Reconstruction in a Pediatric and Adolescent Population
1st Day of #PT after an ACL Surgery
Patella Mobilization after Knee Surgery
Knee Flexion PROM after Surgery- Seated or Supine?
Stretching the Quads after Knee Surgery
Assessing for a Cyclops Lesion after an ACL
Assessing for Fat Pad Irritation of the Knee
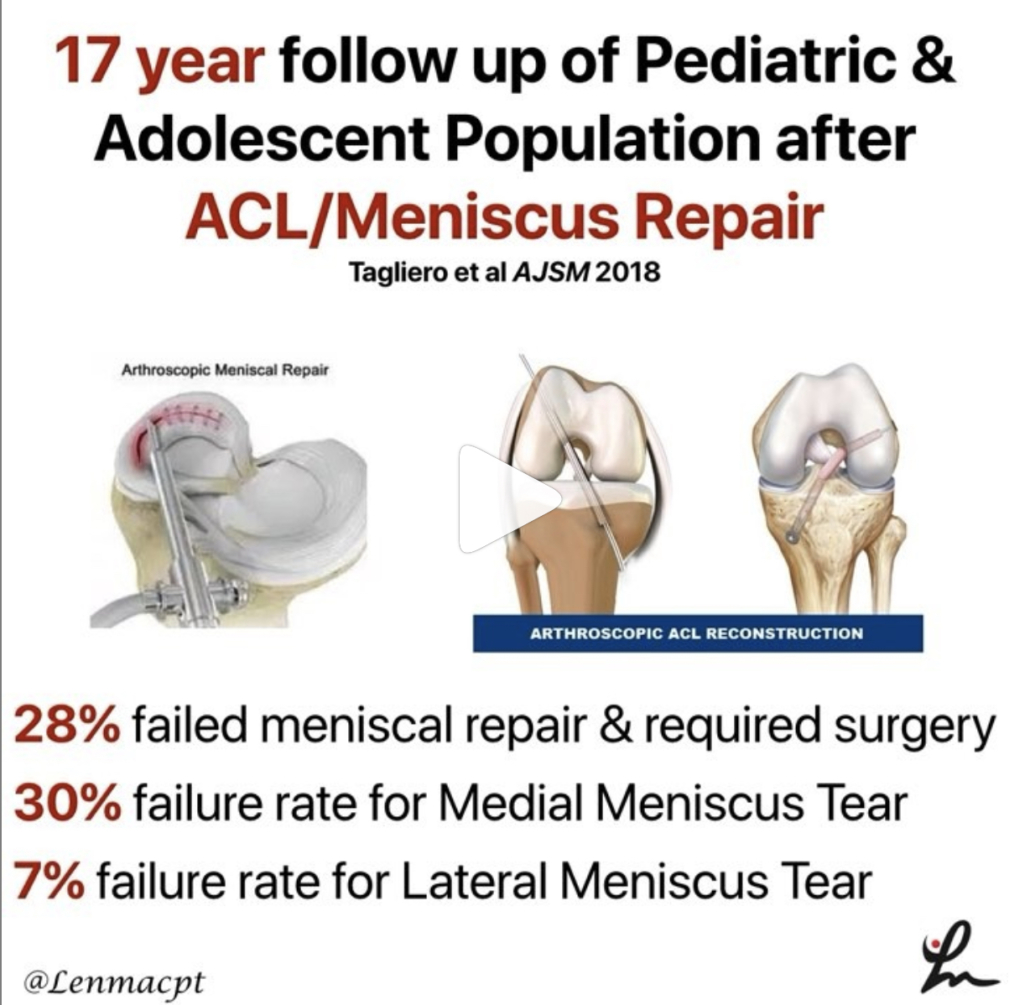
ACL Reconstruction in a Pediatric and Adolescent Population
17 Year Follow-up After Meniscal Repair With Concomitant ACL Reconstruction in a Pediatric and Adolescent Population. Tagliero et al AJSM 2018
Results: 28% failed meniscal repair and required repeat surgery at the time of final follow-up. They also showed that outcomes and failures rates were comparable across tear complexity.
Guess that means that no matter the tear type, there was no difference in outcomes or retear rates. Although the repair techniques are now outdated and no longer used.
Their study also showed a 30% failure rate for meniscal tear repaired in the medial compartment at index surgery and 7% in the lateral compartment.
Interesting long-term outcomes that may help to guide your rehab and client advancement (and prognosis). Keep these in mind when you treat a future adolescent or pediatric ACL patient.
💥1st Day of #PT after an ACL Surgery 💥
If you have never treated a post-op ACL, then this video should interest you!
This is what the knee looks like that 1st day after surgery and can often set the stage for what’s to come over the next 6-12 months.
Often, the patient is both very curious and ultra-grossed out by the 1st unveiling. It can be stressful for them to see their knee in this condition so you really have to confidently reassure them that it is very normal.
The blood-soaked gauze is mainly saline that was used to irrigate the knee during the reconstruction. Some still leaks out of the incisions the 1st few days and can often be confused with true blood.
Understand that this is quite normal and happens to most every ACL patient’s knee that I’ve seen…nothing to worry about!
From here, I’d work on patella mobility (see the post later today) and then work on flexion ROM at the end of the table.
Again, it’s very important to get the knee moving after surgery. This will help with pain, swelling and gain confidence that the rehab process is moving forward.
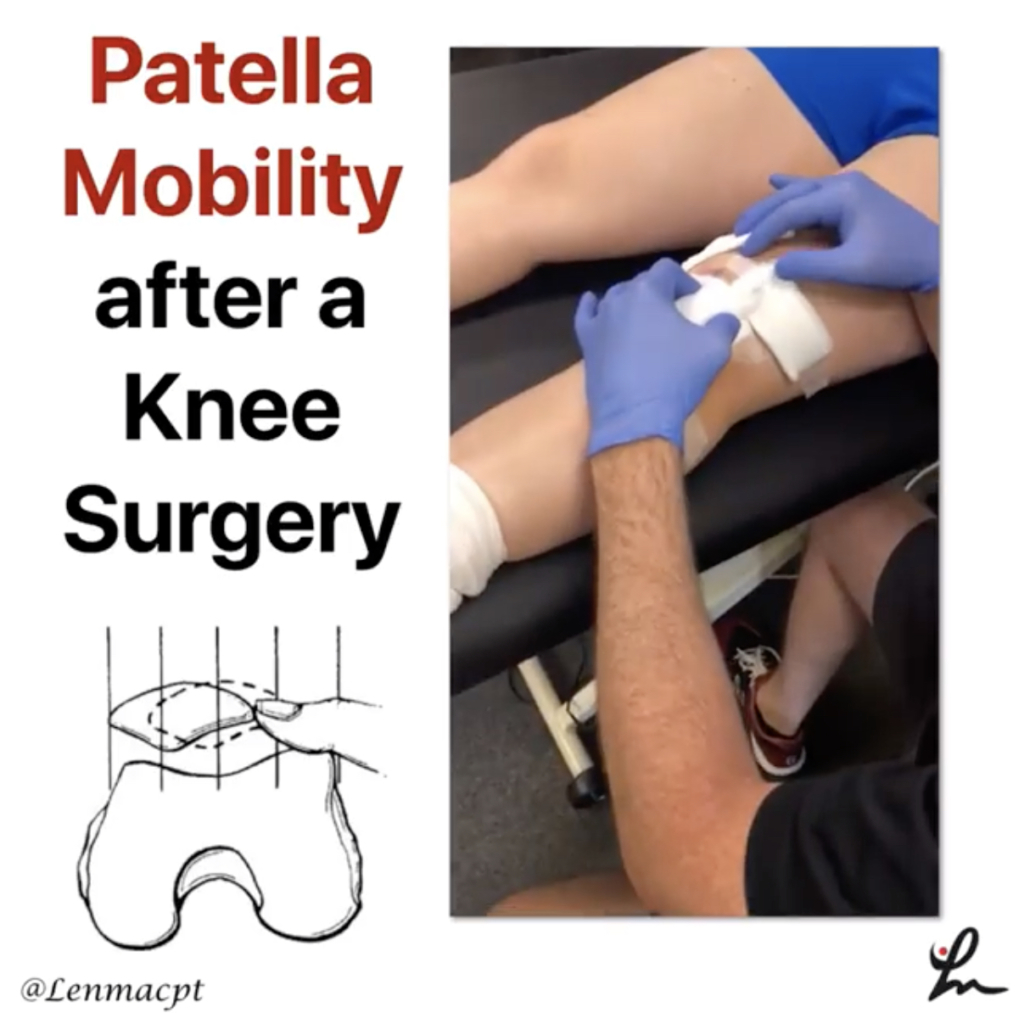
Patella Mobilization after Knee Surgery
Get the patella moving early with #patella mobilizations immediately after surgery. One major reason (amongst many others) why we need to get our clients into #PT early.
I am certainly a very loud advocate for early PT and getting the patella moving can help to prevent excessive scarring, which can affect ROM and quadriceps force output.
Glove up and get that patella moving in all directions… medial, lateral, superior, inferior!
🤔Knee Flexion PROM after Surgery- Seated or Supine? 🤔
I’ve treated many patients after an ACL I can honestly say that this may be a huge influence on the early ROM outcomes that you may see.
I’ve tried to bend the knee in both supine or seated, as the video shows, and there’s no doubt that most people tolerate the seated version so much better after a knee surgery. In particular, a big surgery like an ACL, TKA or MPFL reconstruction.
It just seems to be more comfortable and with less stress on the anterior knee because of the position of the tibia (at least I think so!).
My theory, it seems as if the supine position may cause a slight posterior sag which may cause more pain and guarding than when they’re seated at the edge of the table.
I use a similar concept later on in the rehab process when I’m initiating my prone quad stretching. You can see a definitive improvement when I wedge my hand in the popliteal fossa and create a slight anterior translation on the tibia.
Most people say that the anterior knee pain that they were feeling (and not a quad stretch) was replaced by a stretch feeling only and no more anterior knee pain.
Try it out with your ACL patients and see what position they like best…I’ll bet I can covert you over if you still bend your knee patients in supine!
💥Stretching the Quads after Knee Surgery 💥
Continuing my sequence of videos after a knee surgery, I discussed my technique for progressing knee flexion PROM once they hit 120 degrees or so of flexion.
At this point, they’ve probably maxed out how much ROM they can achieve at the edge of the table. They’re ready to get that end range of motion and even some quadriceps flexibility.
In prone, most people will often feel a pain or pressure in the front of their knee when you try to bend it.
To overcome this, I like to wedge my hand into the back of the knee and give an anteriorly directed force through the gastrocnemius (calf) soft tissue and into the tibia.
This seems to create just enough movement of the tibia on the femur to take the pressure off the front of the knee. This may redirect the forces more onto the quadriceps muscle.
You’ll need to play with the amount and direction of force but most often they’ll begin to feel a better quad stretch.
Try this technique out on your next knee surgery client and see if it helps them. I usually initiate this ~4 weeks after an ACL but timeframes will vary person to person.⠀
💥Assessing for a Cyclops Lesion after an ACL 💥
In this video snippet from my YouTube Channel, I discuss how to assess for a Cyclops lesion in a knee. In particular, after knee surgery.
A patient with a potential cyclops lesion, they often present with loss of normal knee extension compared to the other side. They’ll often have anterior knee pain and poor patella mobility. Sometimes a tight feeling in their hamstrings and calves, too.
No matter how they try to regain their extension ROM, the knee just never feels right. Often times, surgical intervention is needed to remove that scar tissue.
Immediate rehab should continue to work on knee extension ROM using low load long duration stretching and aggressive patella mob’s.
No one’s to blame if this occurs. We don’t know exactly why it occurs in some people but we believe a remnant of the ACL stump may be a source of the frustrating issue.
💥Assessing for Fat Pad Irritation of the Knee 💥
Anterior knee pain is very common in the outpatient #PhysicalTherapy setting.
One of my go-to tests to assess for fat pad irritation is simply trying to capture the fatty tissue in the anterior aspect of the knee joint during active and/or passive ROM.
In this snippet from my YouTube channel, you can see that I pinch the fat pads on either side of the patella tendon as @corrine_evelyn is actively extending her knee. I’ll also do it in a relaxed state to assess passive irritability.
I 1st learned this test from @wilk_kevin and it continues to be a mainstay in my knee examination algorithm.
As for a treatment, it usually comes down to a volume issue and/or strength issue or both.
I’ll usually have to address the volume of the activity by relatively easing off of the activity while simultaneously adding in exercises to address an underlying weakness.
Remember the Dye et al study in AJSM 1998 when he talked about the fat pads being super painful during his arthroscopic surgery without anesthesia. Makes sense why they can be so painful if the knee stresses fall upon this tissue.
We talk about this study, fat pad irritability and much much more in our online knee seminar course.
If you want to learn more about how I treat ACL’s or the knee in general, then you can check out our all online knee seminar at www.onlinekneeseminar.com and let me know what you think.
We cover the anatomy, rehab prescription, ACL, meniscal injuries knee replacements and patellofemoral issues. Furthermore, the course covers both the non-operative and post-operative treatment.t
This is an awesome course if you’re interested in learning more about rehabilitating the knee joint. And if you’re a PT, there’s a good chance you can get CEU’s as well.