Anterior Knee Pain- A Test for Fat Pad Irritation
We as physical therapists are constantly seeing patients with anterior knee pain with a very vague history. Often times, there’s not a specific onset or mechanism of injury. With that, it seems as if the retro patellar fat pad is a common source of pain in many people and is commonly overlooked.
What actually hurts in the knee?
Whenever I am evaluating someone with knee pain, I always keep in mind the Dye et al AJSM article from 1998. In my opinion, this is a keeper for all PT’s and future PT’s to have in their arsenal of top literature papers.
For those that are not familiar, let me explain it a bit.
Basically, San Francisco orthopaedic surgeon Dr. Scott Dye had his knee scoped without any anesthesia. That’s right, classic beast mode!
He did have local anesthesia (for the record), so they could make the incisions…otherwise, he was awake and alert for the whole procedure.
This allowed him to report back to his colleagues (one being his brother) an actual pain response as they were poking away at the different structures within the knee. He ranked the pain on a 0-4 scale with 0 being pain-free (patella cartilage) and 4 being a severe pain (fat pad, anterior synovium, joint capsule.)
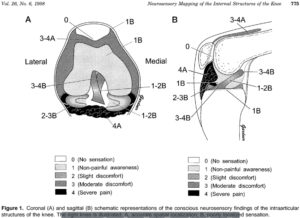
You can read the article to get the full gist (and I HIGHLY RECOMMEND this!) but my point is to let you realize that there are only certain structures capable of causing severe pain in the anterior knee.
Their Findings
Cartilage is avascular and aneural. It has no blood supply or nerves that innervate it. None! So the whole chondromalacia patella diagnosis attempting to implicate a maltracking patella is often hogwash.
But the fat pad, anterior synovium, and anterior capsule are extremely painful and are often involved, I believe, in patients that we see on a daily basis.
In my opinion, this is a diagnosis that sees us more than we see it. Like thoracic outlet syndrome… we can talk about that a different day though.
Back to the point of the blog.
1 Test for Fat Pad Assessment
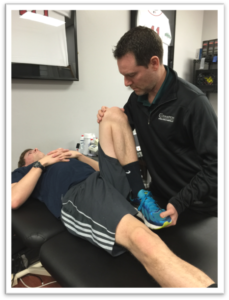
Assessing the knee and asking the right questions is critical. Besides a tremendously great subjective, there’s one test that I use to rule in or out a fat pad irritation. Check out the video below:
I promise you this test is a great way to establish a pretty clear diagnosis and reassure the patient that a specific structure may be the issue.
When it’s painful, its pretty obvious and the patient can immediately report back to you their symptoms. I test for this a bunch in a given week and it’s not always present. But when someone presents with a positive finding, it’s pretty relieving to them (believe it or not.)
Differential Diagnosis
Keep in mind, my differential diagnosis is all over the place at times. With knee pain you need to consider:
- Meniscus (see my previous blog post)
- ITB
- Osteochondral lesion
- Patella tendonitis
- Pes anserine bursitis
- MPFL sprain
- Hamstring strain
- Plica syndrome
- MCL/LCL
- Tumor
That’s a bunch to consider for someone who can’t really explain why or when their injury occurred. That’s why I still believe this overuse injury sees us more than we see it.
Treatment of Fat Pad Irritation
This one can get a bit tricky. Again, it’s often due to an overuse injury. In others, it’s attributed to kneeling on it for too long or banging it against something. In those more acute cases, the answer is pretty straightforward. Ice, motion and progressive return to their function.
In the overuse group, which is more prevalent in my opinion, we need to figure out which stimulus is causing the issue. It’s often due to starting a new program or ramping up too quickly during some training event.
In these people, I need to modify their volume of training or destress the area by giving them new activities that they can do pain-free…but only for a short period of time.
Along with activity modification, a course of some form of modality (yup, the M-word was used) can help expedite the pain control. I still have a special place in my heart for iontophoresis with dexamethasone. I’ve had tremendous results in patients with fat pad irritation.
I also like to use a low-level laser to help with the healing process (future blog post alert!) I’ve used it on my self for various ailments and even my dog after her ACL surgery. I’m definitely a believer in the healing power of the laser when applied in the correct situation.
Besides all of that, I would also want to assess the person’s movements and attempt to adjust any motions or movements that I thought could contribute to the knee pain. Often times, there’s an underlying weakness or misconception of a weakness that needs to be explained to the patient.
These things run their course for a few weeks but should improve pretty quickly if handled correctly. Patient gratification is pretty obvious because their pain diminishes after a session or 2 and they buy into the program pretty quickly.
Fat Pad Conclusions
Infrapatellar fat pad irritation can be functionally debilitating. I believe it presents itself pretty often in the clinic, more than most PT’s realize. Use my test above to see if it truly is a fat pad issue. Here’s a nice open-access article that you can read to learn more about the fat pad.
Remember, the test should be pretty obvious and locally oriented. If pain-free, then move on. If not, then try some of my above recommendations. It’s usually an overuse issue so you need to adjust their volumes and maybe some form of mechanics.
Mike Reinold and I discuss this and much more about how we treat the knee conservatively. Check it out in our acclaimed all online knee course www.onlinekneeseminar.com.