Diagnosing meniscus tears: What’s the literature telling us now?
Meniscal tears are commonly observed in an outpatient physical therapy setting. The ability of a PT to evaluate a patient’s knee and diagnose a meniscus tear can help guide the treatment plan for that patient. Having specific tests that can accurately and quickly pick up a meniscal tear are valuable.
Lots of test options but stick with the subjective
There are many theories, tests, and exam techniques that are reported in the literature. I definitely don’t know all of them but have been exposed to a bunch of common ones that I have found to be helpful.
Before I get bogged down with these tests and try to sound intelligent, I’d be remiss to not state the obvious… the subjective portion of the exam is by far the most important aspect and needs to be thoroughly utilized. In many cases, ok maybe most cases, the client will tell you what’s going on…as long as you ask the questions correctly and listen to their responses.
This will most likely be a blog post at some point in the near future but as a collective profession known as medicine, we suck at listening and utilizing the information correctly. But I digress…
What Tests are out there?
There are many tests reported in the literature, commonly including:
- McMurray’s
- Apley’s compression
- Joint line tenderness
- Thessaly’s
- End range flexion/extension overpressure
Unfortunately, the literature does not support using these tests to diagnose and may add to the fear avoidance a patient may exhibit after such a diagnosis. This systematic review and meta-analysis in the British Medical Journal stated:
“The results of this systematic review indicate that the accuracy of McMurray’s, Apley’s, JLT and Thessaly to diagnose meniscal tears remains poor. This conclusion must be taken with caution since frequent methodological design flaws exist within the included studies, most studies suffered from various biases, and between-study heterogeneity makes pooled data unreliable.”
To tell you the truth, I don’t even do the Apley’s compression test. I probably haven’t done the test since PT school sometime in 2001. Never saw a value, kinda like the Thessaly Test. Nice in theory but just not good enough when tried in a clinical setting. Unfortunately, most research and the associated methods are lacking so the results are pretty poor when trying to diagnose a meniscus tear.
Oh boy, now what do we do? Do we even need to diagnose the tear in the 1st place and add more fear to the patient’s hurting knee?
Even need to Diagnose Meniscus Tears?
I say yes… but with a caveat!
We must accurately diagnose and explain to the patient that many people have meniscal tears in their knee. The recent literature builds a strong case for a very good recovery without surgery. That’s right, surgery is often not needed for many people diagnosed with a meniscus tear.
This landmark paper in the New England Journal of Medicine (neighbors of Champion PT and Performance in Waltham, MA) really created waves when it was released in 2013. They stated that “outcomes after arthroscopic partial meniscectomy were no better than those after a sham surgical procedure.” Now, these people did have a diagnosis of knee arthritis as well, but so do many of the people we see on a daily basis.
Hopefully, many clinicians have changed their treatment algorithms and have opted for conservative treatment first.
Don’t get me wrong, surgery may be needed, especially for the people sustaining an acute meniscus tear. But that may only be a small portion of the people presenting to us in the clinic. In these people, I still say give it a bout of conservative treatment to calm the knee down, restore ROM and strength and see how they do. Maybe a 6 week PT course is all they need, you never know. I have definitely seen it work, no doubt!
What meniscus tests do I do?
With all of that being said, I still believe your clinical examination is ultra-important to help guide the treatment plan.
As usual, keep it simple and don’t over-search. It needs to be pretty straightforward and it often is. The exam NEEDS to match the clinical history…let me say that again….the exam NEEDS to match the clinical history.
The client is going to tell me their issue and I just need to make sure my tests and measures solidify my working theory. I promise you that if you ask the right questions the right way, then you will have that much more information to at your disposal.
So, my go-to tests are:
- Joint line palpation
- End range flexion/extension pain/locking
- McMurray’s (but often not very valuable)

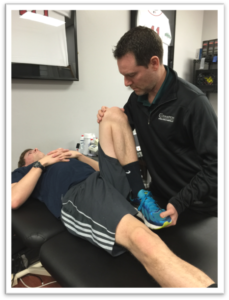

…in that order. I’d say joint line palpation and end range of motion are my 2 most valuable tests. I still do the McMurray’s test to see if it can add to the story. It often gives me very little information so I don’t rely on it too much.
Many of you are going to ask why I didn’t even mention the Thessaly test. I see it talked about a lot on social media. I just don’t understand why we’d want to put our client in a weight-bearing position, slightly bend their knee, and have them twist on a painful knee.
Never mind the research telling us that the test is not very valid which goes completely against early research that said it was a valid test.
The more (tests) the Merrier
Maybe we need to combine this test with others to help improve our accuracy as this paper showed in 2009.
Either way, there seems to be a case to cluster tests to help us draw better conclusions, as was stated in this paper in 2006. “Five positive findings on composite examination yielded a positive predictive value of 92.3%. Positive predictive values remained greater than 75% with composite scores of at least 3 in the absence of ACL and DJD pathologies.”
This paper nearly matches my thought process. Obtain a good history, assess the joint line for tenderness, then put the joint at end range flexion/extension. If the symptoms match, then we will OFTEN have a meniscus tear.
Keep in mind that the particular side of the meniscus tear may influence the ability to detect a pathology. Lateral meniscal tears may be easier to distinguish than medial meniscal tears if we’re talking about joint line tenderness alone and was even the case in this 2009 article too.
Final Word on Diagnosing Meniscus Tears
Meniscus tears are pretty prevalent in the outpatient setting. Rehab specialists, including PT’s and athletic trainers need to understand what tests are best to deploy. I’m sticking with my in-depth history, joint line tenderness, and painful end-range as my go-to cluster of tests.
I’m pretty sure it has done me well over the years…and the research seems to match my thoughts too.
Online Knee Seminar Course
We discuss this and much much more in my online knee course that I have with Mike Reinold. If interested, check it out at www.onlinekneeseminar.com and let me know what you think. We cover the anatomy, rehab prescription, ACL, knee replacements and patellofemoral issues both non-operative treatment and post-operative treatment. This is an awesome course if you’re interested in learning more about rehabilitating the knee joint.

