Looking back at 2017 & beyond to 2018
It’s that time of year to reflect on what we’ve done and a game plan on what’s to come. I’ve taken a moment to look back at some changes I made in 2017 and share it with you.
New website- LennyMacrina.com

I had been thinking about building my website for a while. Being surrounded by some of the guru’s in our field, who have used their website to share their thoughts, I had no choice but to take the leap.
Mike (mikereinold.com), Dave (shiftmovementscience.com), and Dan (Fitnesspainfree.com) are constantly talking about WordPress, funnels, and calls to action than most. As much as it’s gibberish, it made me think about why I don’t have my own calling card, so to speak, to be able to capture my opinions on rehabilitation and physical therapy.
I fumbled a bunch and had to redo the whole site from scratch after hiring someone to do it for me. In the meantime, I had to develop knowledgeable content that people may find interesting.
Instead of just using my Twitter (@lenmacpt), Facebook (Lenny Macrina MSPT, SCS, CSCS) or Instagram (@lenmacpt) accounts to share content, I decided to centralize the process. I figured this would be my home base for content that I can control forever and not be stuck in a social media platform.
I feel like I’m winging it but the early feedback has been pretty positive.
Improve my Listening Skills
I’ve said over and over again that listening to your clients is the most important aspect of any examination.
I feel as if I do a pretty good job at listening to my clients (despite what my wife says about my listening skills.) I try to ask the right questions and let the client state their story. Too often we get ideas in our head and jump to conclusions. We try to diagnose an injury too quickly and may miss an important detail that could sway the story in a different direction.
I’ve had this happen numerous times and completely blame myself for not giving the client the platform to reveal the pertinent details. I alluded to this is in a previous post if you’re interested. The client comes first…no questions asked!
Remember, they don’t know what may be contributing to their injury. To them, the injury is often a result of a specific action. They don’t consider the other contributing factors in their lives that seem insignificant.
I always ask them “What do YOU think is going on?” This allows me to hear their thoughts, impressions and any details that they think may be adding to their current presentation
For example, I recently had a client present with shooting and burning pain down her arm. To many, it would seem like a cervical herniated disk. Pretty clear cut, right?
Well, she had a clavicle fracture that required an ORIF 10 years ago. She didn’ think it was significant but every time I palpated at the surgical site, especially the lateral aspect, we could replicate her symptoms…Every time! Two previous medical professionals missed this detail and just brushed it off.
To me, it seemed pretty clear that some component of her ORIF or clavicle had been rubbing a portion of her brachial plexus during a specific movement. It just did not seem like a cervical spine issue and the detail of her clavicle fracture, that she thought was insignificant, seemed to be the clue we needed to hone in on the culprit.
Listen up…they may just tell you what you need to hear!
Systemize Everything
Life gets crazy. Responsibilities grow so we need a way to manage all of the chaos. What helped me to better manage my time was contained in the book “15 Secrets Successful People Know About Time Management: The Productivity Habits of 7 Billionaires, 13 Olympic Athletes, 29 Straight-A Students, and 239 Entrepreneurs“
I’ve had to block time out of my calendar to get tasks done. Like specific times to do specific tasks. Whether it’s a dentist appointment, a powerpoint or running payroll, I have reminders in my calendar for everything.
More importantly, I have to prioritize tasks, what Kevin refers to as my MIT’s or Most Important Tasks.
I have done my best to stick with this plan but he recommends working on your MIT 1st thing in the morning when he thinks you are the sharpest. As of now, I have carved this time out to be with my daughter before the day begins. I guess as of writing this, she is my most important task. Can’t argue that!
At work, including client evaluation and treatment sessions, we have begun to systemize everything we do at Champion PT and Performance. We feel as if most people present with very similar presentations.
We’ve developed internal treatment progressions that we utilize daily. It makes it a lot easier for PT’s to see each other’s clients on the rare occasion we need to cover for someone. It takes any questions out of the client’s head. They don’t need to worry why their regular PT may or may not be doing a specific treatment.
Even more than that, we MAY have a new system coming out in 2018 that will help many with their evaluation skills. I can’t say much more than that but look for a big announcement mid-2018!
Preview of 2018
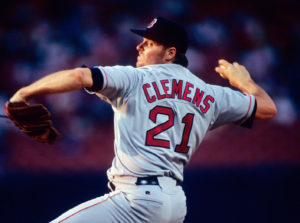
Wow, 2018 is right around the corner. I feel good about it because it’s an even number. Yeah, I’m a bit weird with stuff like that. Maybe it’s my baseball background and superstitions.
- In 2018 I hope to accomplish more vlogs…or video blogs as the kids say. I feel like a 3-5 minute snippet of my thoughts is a very effective way of communicating with the masses. Look for more vlogs as we roll into luck 2018.
I also plan on booking more speaking engagements worldwide. As of now, my calendar has me in:
- Birmingham, AL for ASMI’s Injuries in Baseball Course. Following that, I’ll be in
- Portland, OR for the Pacific NW Orthopedic and Sports Medicine Symposium in early April.
- While in the great northwest, I’ll swing by my old friends at Medbridge to record a course on Baseball Injuries for their SCS prep courses.
- June takes me over to Paris, France for a 2-day course on Shoulder Rehabilitation. Looking forward to taking the roadshow internationally.
- October takes me back to Canandaigua, NY with my co-worker Kiefer Lammi. We’re teaching a 1-day strength and conditioning integrated course for their local PT’s within their health system.
I have other courses that just need to be finalized but it seems like there may be 1-2 more dates that are in the works.
2018 is shaping up to be a very exciting and productive year. It’s important that I have these plans in place to keep me on my toes and on top of the literature.
Hope you have looked back at your past year and can continue to build into 2018. What goals do you have for 2018? Hit me up in the comments below so we can discuss.
Happy New Year!!